Spinal fractures can be debilitating, causing severe pain and limiting mobility. Vertebroplasty is a minimally invasive procedure used to treat painful spinal fractures, particularly those caused by osteoporosis, trauma, or tumors.
In this article, we’ll explore everything from the causes and symptoms of spinal fractures to the vertebroplasty procedure, its benefits, risks, and the recovery process.
In This Article:
- Key Takeaways
- Understanding Spinal Fractures
- The Vertebroplasty Procedure
- Benefits of Vertebroplasty
- Risks and Complications
- Recovery and Rehabilitation
- Is Vertebroplasty Right for You?
- FAQs
- What is vertebroplasty?
- Who is a good candidate for vertebroplasty?
- How long does the vertebroplasty procedure take?
- What is the recovery time after vertebroplasty?
- What are the benefits of vertebroplasty?
- What are the risks and complications of vertebroplasty?
- Is vertebroplasty painful?
- How long does the pain relief from vertebroplasty last?
- Can vertebroplasty prevent future fractures?
- What are the alternatives to vertebroplasty?
- Conclusion
- Novus Spine & Pain Center
- Resources
Key Takeaways
- Effective Pain Relief: Vertebroplasty provides immediate and significant pain relief for patients suffering from vertebral compression fractures.
- Improved Spinal Stability: The procedure strengthens and stabilizes the fractured vertebra, reducing the risk of further collapse and deformity.
- Enhanced Quality of Life: Vertebroplasty alleviates pain and improves mobility, enabling individuals to regain their independence and enjoy a better quality of life.
- Minimally Invasive: Vertebroplasty is a minimally invasive procedure with a short recovery time, allowing patients to return to their daily activities sooner.
- Potential Risks: While generally safe, vertebroplasty carries the possible risks of cement leakage, infection, and nerve damage. Choosing an experienced provider is crucial.
- Not a Preventive Measure: Vertebroplasty treats existing fractures but doesn’t prevent future ones. Addressing underlying causes like osteoporosis is essential.
- Consult Your Doctor: If you’re experiencing pain from a vertebral compression fracture, consult your doctor to discuss if vertebroplasty is right for you.
Understanding Spinal Fractures
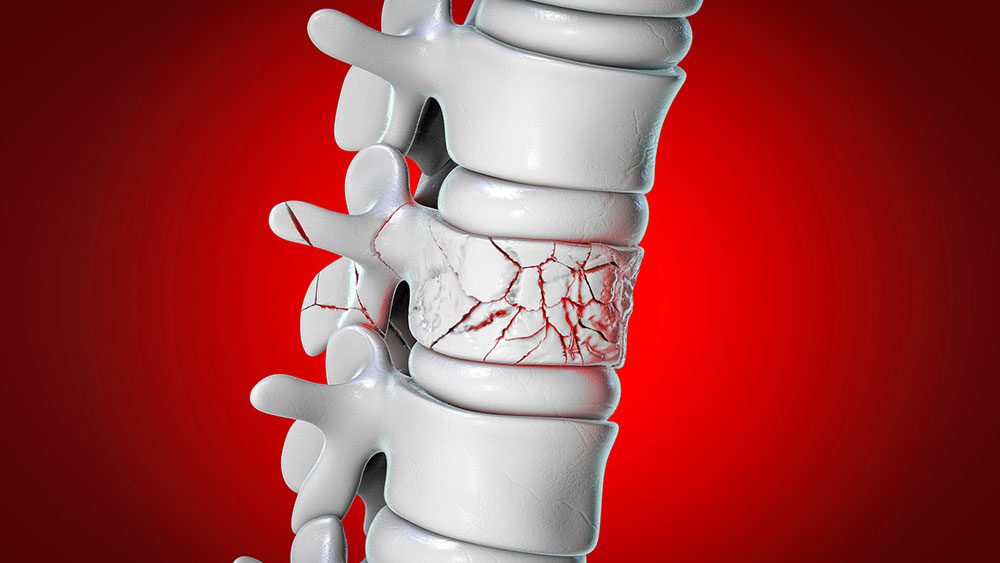
Spinal fractures, also known as vertebral fractures, occur when one or more of the bones in your spine break or collapse. These breaks and fractures can cause significant pain, limit mobility, and impact your overall quality of life. Understanding spinal fractures’ common causes and symptoms is important when seeking a diagnosis and treatment.
Common Causes of Spinal Fractures
Multiple factors can play a role in the development of spinal fractures.
- Osteoporosis. A condition that weakens the bones, making them more susceptible to fractures, even from minor stresses or falls.
- Trauma. High-impact injuries from car accidents, falls, or sports-related incidents can cause fractures in the spine.
- Tumors. Cancerous or benign tumors can weaken the spinal bones, increasing the risk of fractures.
Symptoms of Spinal Fractures
Recognizing the signs of a spinal fracture is crucial as this will help in seeking immediate medical attention. A list of common symptoms includes:
- Back Pain: Sudden or gradual onset of back pain, often worsened by movement or activity.
- Loss of Height: Compression fractures can cause the spine to collapse, leading to a noticeable decrease in height.
- Spinal Deformity: In severe cases, fractures can result in a visible curvature or hump in the back.
If you experience any of these symptoms, it’s crucial to consult with a pain doctor for evaluation and diagnosis. Early detection and treatment can help prevent further complications and improve the chances of a successful recovery.
The Vertebroplasty Procedure
Vertebroplasty is a minimally invasive procedure typically performed on an outpatient basis. It involves injecting bone cement into the fractured vertebra to stabilize it and help provide pain relief. Let’s delve deeper into the steps involved in this procedure.
Preparation for the Procedure
Before the vertebroplasty procedure, you will undergo several preparatory steps:
- Imaging Tests: Your doctor will use imaging tests, such as X-rays, CT scans, or MRIs, to pinpoint the fracture’s exact location and severity.
- Anesthesia: You will receive local anesthesia to numb the area around the injection site, ensuring a comfortable experience during the procedure. In some cases, you may opt for conscious sedation to help you relax.
Step-by-Step Guide to Vertebroplasty
The vertebroplasty procedure itself is relatively straightforward. Using imaging guidance, your doctor carefully inserts a thin needle into the fractured vertebra. Once in place, a special bone cement, typically polymethylmethacrylate (PMMA), is injected into the vertebra.
The cement hardens quickly, stabilizing the fracture and providing immediate pain relief in most cases.
Post-Procedure Care
After the vertebroplasty, you will be monitored for a short period before being discharged. Here’s what you can expect in terms of post-procedure care:
- Recovery Time: Most patients experience significant pain relief immediately after the procedure and can go home the same day.
- Activity Restrictions: Your doctor may advise you to avoid strenuous activities or heavy lifting for a few days until the special cement fully hardens.
Vertebroplasty is a safe and effective procedure with a high success rate in relieving pain and improving spinal stability. However, as with any medical procedure, there are potential risks and complications, which we will discuss in the next section.
Benefits of Vertebroplasty
Vertebroplasty offers a range of benefits that make it an appealing treatment option for individuals suffering from painful vertebral compression fractures. These advantages contribute to improved quality of life and overall well-being.
Pain Relief
The most immediate and significant benefit of vertebroplasty is its ability to provide rapid and substantial pain relief. The procedure alleviates pressure and irritation on surrounding nerves by stabilizing the fractured vertebra with bone cement, significantly reducing or eliminating pain.
Many patients experience immediate relief, allowing them to regain mobility and engage in daily activities more easily.
Improved Spinal Stability
Vertebral compression fractures can compromise the structural integrity of the spine, leading to instability and an increased risk of further fractures. Vertebroplasty addresses this issue by reinforcing the weakened vertebra with bone cement, restoring its strength and preventing further collapse. This enhanced stability contributes to improved posture, reduced risk of future fractures, and greater confidence in movement.
Enhanced Quality of Life
The combined effects of pain relief and improved spinal stability can significantly enhance overall quality of life. Individuals are able to resume their daily activities, hobbies, and social engagements with reduced pain and increased mobility. The ability to move freely and comfortably without chronic pain can have a profound impact on the patient’s emotional and psychological well-being. It can also foster a more positive outlook and a greater sense of independence.
Vertebroplasty’s minimally invasive nature adds to its appeal. It typically involves a shorter recovery time than more extensive surgical procedures, allowing patients to return to everyday activities sooner and minimizing disruption to their lives.
Moreover, the procedure is commonly conducted on an outpatient basis, eliminating the need for hospitalization.
Risks and Complications
While vertebroplasty is generally considered a safe and effective procedure, it’s essential to be aware of the potential risks and complications that may arise.
Potential Risks
Although rare, some of the potential risks associated with vertebroplasty include:
- Cement Leakage: In some cases, bone cement may leak out of the vertebra and into surrounding areas, potentially causing nerve compression or other complications.
- Infection: As with any surgical procedure, there is a slight risk of infection at the injection site.
- Nerve Damage: Although uncommon, nerve damage can occur if the needle used during the procedure accidentally contacts a nerve.
Importance of Choosing an Experienced Provider
The skill and experience of the healthcare professional performing the vertebroplasty play a crucial role in minimizing the risks and ensuring a successful outcome. Choosing a qualified and experienced pain doctor with a proven track record in performing this procedure is essential.
It’s also important to remember that the benefits of vertebroplasty often outweigh the risks for most patients. However, it’s crucial to have an open and honest discussion with your pain doctor about the potential complications and ensure that you are a suitable candidate for this procedure.
Understanding the risks can help you decide whether vertebroplasty is the right treatment option for your spinal fracture.
Recovery and Rehabilitation
After undergoing vertebroplasty, you can expect a relatively quick recovery with minimal downtime. However, adhering to your doctor’s recommendations and engaging in rehabilitation exercises can help optimize your healing process and ensure a smooth return to your normal daily activities.
Typical Recovery Timeline
Most patients experience significant pain relief immediately after the vertebroplasty and can return home the same day. However, while the bone cement fully hardens, you may need to rest for a few days and avoid strenuous activities.
Physical Therapy and Exercise
Your doctor may recommend physical therapy to help you regain strength, flexibility, and mobility in your spine. A physical therapist can guide you through specific exercises and stretches tailored to your needs and recovery progress.
Returning to Normal Activities
The timeline for returning to your normal activities will vary depending on your circumstances and the severity of your fracture. However, most patients can gradually resume their daily routines within a few weeks of the procedure.
It is essential to listen to your body and avoid overexerting yourself during recovery. If you experience any pain or discomfort, communicate with your doctor or physical therapist.
By following the recommended recovery and rehabilitation plan, you can maximize the benefits of vertebroplasty and enjoy a faster, more complete recovery.
Is Vertebroplasty Right for You?
Vertebroplasty offers significant benefits for many patients suffering from painful spinal fractures. However, it’s crucial to determine whether it’s the most suitable treatment option for your specific condition and circumstances.
The first step in determining if vertebroplasty is right for you is to consult a pain doctor for a thorough evaluation. The assessment will include a review of your medical history, physical examination, and imaging tests to assess if vertebroplasty is the correct procedure for you.
Factors to Consider
Several factors will be considered when determining if vertebroplasty is appropriate for you:
- Type of Fracture: Vertebroplasty is most effective for compression fractures caused by osteoporosis, trauma, or tumors.
- Overall Health: Your health and any pre-existing medical conditions will be evaluated to ensure you can safely undergo the procedure and anesthesia.
- Expectations: It’s important to have realistic expectations about the outcomes of vertebroplasty. While it can help relieve pain and improve spinal stability, it may not eliminate all discomfort or restore full mobility.
If you’re experiencing persistent back pain due to a spinal fracture, don’t hesitate to discuss vertebroplasty with a pain doctor who can help you weigh the potential benefits and risks. Your doctor can help you decide the most appropriate treatment path for your needs.
FAQs
What is vertebroplasty?
Vertebroplasty is a minimally invasive medical procedure designed to treat painful vertebral compression fractures, which are common in people with osteoporosis or those who have experienced trauma or tumors in the spine. During this procedure, a special bone cement is injected into the fractured vertebra with the aid of imaging guidance. The cement hardens quickly, stabilizing the fracture and providing immediate pain relief.
Vertebroplasty aims to restore the structural integrity of the affected vertebra, reducing pain and improving mobility. It’s typically performed on an outpatient basis, allowing patients to return home the same day. This procedure offers a viable solution for individuals seeking a quick and effective way to manage pain and enhance their quality of life following a spinal fracture.
Who is a good candidate for vertebroplasty?
Vertebroplasty is primarily recommended for individuals experiencing significant pain and reduced mobility due to vertebral compression fractures. These fractures often occur as a result of osteoporosis, trauma, or tumors affecting the spine.
Ideal candidates for vertebroplasty typically have:
- Recent Fractures: The procedure is generally most effective when performed within a few weeks to a few months after the fracture occurs.
- Persistent Pain: Candidates should have pain that hasn’t improved with conservative treatments like rest, pain medication, or physical therapy.
- Specific Fracture Locations: Vertebroplasty is most suitable for treating fractures in the thoracic and lumbar spine (mid- and lower back).
- No Neurological Symptoms: Candidates shouldn’t have signs of spinal cord compression or nerve damage, which might require different treatment approaches.
It’s important to consult with your pain doctor to determine if vertebroplasty is the right option for you. The doctor will assess your specific symptoms and medical history to recommend the best treatment options.
How long does the vertebroplasty procedure take?
The vertebroplasty procedure is relatively quick, typically taking 30 minutes to an hour per fractured vertebra being treated. However, the total time spent at the medical facility may be longer, including preparation, anesthesia administration, and post-procedure monitoring.
Factors that can influence the overall duration include the number of vertebrae needing treatment, the complexity of the fractures, and any individual patient considerations. While the procedure is efficient, allocating ample time for the entire process is essential to ensure a safe and successful outcome.
What is the recovery time after vertebroplasty?
Vertebroplasty has a relatively quick recovery period, with most patients experiencing significant pain relief almost immediately after the procedure. You can typically go home the same day and resume light activities in 24 hours. However, avoiding strenuous activities or heavy lifting for several weeks is crucial to allow the bone cement to harden fully and the fracture to stabilize.
While some soreness at the injection site is normal, it usually subsides within a few days. Most individuals can return to regular routines, including work and daily activities, within a few weeks. However, the exact timeline can vary depending on the severity of the fracture and individual healing rates. Following all post-procedure instructions and attending recommended physical therapy sessions is crucial to optimizing recovery and ensuring long-term success.
What are the benefits of vertebroplasty?
Vertebroplasty offers several key benefits for individuals suffering from painful vertebral compression fractures:
- Immediate Pain Relief: One of vertebroplasty’s most significant advantages is its ability to provide rapid and substantial pain relief. Many patients experience a significant reduction in pain almost immediately after the procedure, allowing them to regain mobility and improve their quality of life.
- Improved Spinal Stability: By injecting bone cement into the fractured vertebra, vertebroplasty strengthens and stabilizes the bone, preventing further collapse and deformity. This can lead to improved posture, reduced risk of future fractures, and enhanced overall spinal health.
Additionally, vertebroplasty is a minimally invasive procedure with a short recovery time, allowing patients to return to their daily activities sooner compared to more extensive surgical interventions.
What are the risks and complications of vertebroplasty?
While vertebroplasty is generally considered a safe procedure, it’s important to be aware of potential risks and complications. The most common complication is cement leakage, where some of the injected cement seeps out of the targeted vertebra.
In most cases, any leakage is minor and doesn’t cause any issues. However, if the cement leaks into the spinal canal or presses on nerves, it can lead to new or worsened pain, numbness, or weakness.
Other less common risks include infection at the injection site, bleeding, nerve damage, and allergic reactions to the cement or anesthesia. In rare cases, the cement can enter the bloodstream and travel to the lungs, heart, or brain, potentially causing serious complications. Discussing these risks with your pain doctor before the procedure is crucial.
Is vertebroplasty painful?
Vertebroplasty is generally not considered a painful procedure. You will receive local anesthesia to numb the area where the needle is inserted, and you may also be given medication to help you relax during the procedure. Some patients report feeling mild pressure or discomfort during the injection of the bone cement, but it is usually well-tolerated.
After the procedure, you may experience some soreness at the injection site, which can be managed with over-the-counter pain medications or ice packs. The pain associated with the fractured vertebra should be significantly reduced or eliminated almost immediately after the procedure, offering substantial relief and improving your overall comfort.
How long does the pain relief from vertebroplasty last?
One of the most remarkable aspects of vertebroplasty is its ability to provide immediate and significant pain relief. Many patients report feeling a noticeable reduction in pain right after the procedure. This immediate relief can be life-changing, allowing individuals to regain mobility and enjoy a better quality of life.
While the initial pain relief is often rapid, the long-term duration can vary depending on several factors, including the underlying cause, the severity of the fracture, and the patient’s overall health. Studies suggest that most patients experience sustained pain relief for at least one year, with some individuals reporting benefits for several years.
It’s important to remember that while vertebroplasty addresses the pain associated with the fracture, it doesn’t treat the underlying condition that caused the fracture in the first place. Therefore, following your doctor’s recommendations for managing any underlying conditions, such as osteoporosis, is essential to minimize the risk of future fractures.
Can vertebroplasty prevent future fractures?
Vertebroplasty treats existing fractures and provides pain relief rather than preventing future fractures. While the procedure strengthens and stabilizes the treated vertebra, it doesn’t address the underlying cause of the fracture, such as osteoporosis.
However, by stabilizing the fractured vertebra, vertebroplasty can indirectly help reduce the risk of future fractures in the same area. Restoring the vertebra’s height and alignment helps maintain proper spinal mechanics and reduces stress on adjacent vertebrae.
It’s crucial to remember that addressing the underlying cause of the fracture, such as osteoporosis, through medication, lifestyle changes, and other treatments is essential for preventing future fractures in other areas of the spine.
What are the alternatives to vertebroplasty?
If vertebroplasty isn’t suitable for your situation or you’re seeking other treatment options, there are several alternatives for managing painful vertebral compression fractures.
- Conservative Management: For mild fractures or those causing minimal pain, conservative treatments like rest, pain medications, physical therapy, and bracing may be sufficient to manage symptoms and promote healing.
- Kyphoplasty: Similar to vertebroplasty, kyphoplasty involves injecting bone cement into the fractured vertebra. However, kyphoplasty also utilizes a balloon to create a cavity within the vertebra, aiming to restore some of its lost height.
- Spinal Fusion: In cases where multiple vertebrae are fractured, or significant instability is present, spinal fusion surgery may be recommended. This procedure involves joining two or more vertebrae to create a solid bone mass, providing stability and reducing pain.
It is crucial to discuss these alternatives with your pain doctor to determine the most appropriate course of action based on your specific condition, overall health, and personal preferences.
Conclusion
Vertebroplasty offers a promising solution for individuals suffering from painful spinal fractures. Stabilizing the fractured vertebra and providing pain relief can significantly improve the patient’s quality of life. If you are experiencing back pain due to a spinal fracture, consult with your pain doctor to discuss whether vertebroplasty is a suitable treatment option.
Remember, early diagnosis and treatment are vital in managing spinal fractures effectively. You can take a proactive step towards regaining your strength, mobility, and overall well-being by seeking timely medical advice and exploring treatment options like vertebroplasty.
Novus Spine & Pain Center
Novus Spine & Pain Center is in Lakeland, Florida, and treats patients with chronic pain with numerous therapies, including vertebroplasty. By using a comprehensive approach and cutting-edge therapies, we work together with patients to restore function and regain an active lifestyle while minimizing the need for opiates.
For your convenience, you may schedule an appointment online, request a call back, or call our office at 863-583-4445.
Additional Resources
Vertebroplasty (Mayo Clinic)
Vertebroplasty (Johns Hopkins)
Vertebroplasty (Cleveland Clinic)
Vertebroplasty Procedure (Spine-Health)

