 Osteoporosis is a disease that causes bones to become fragile and easily break, especially the bones in the hip, spine, and wrist. The most serious and debilitating osteoporotic fracture is a hip fracture. Men and women over the age of 60 are at higher risk of osteoporosis than younger people. Nevertheless, it is possible to have osteoporosis at a much earlier age.
Osteoporosis is a disease that causes bones to become fragile and easily break, especially the bones in the hip, spine, and wrist. The most serious and debilitating osteoporotic fracture is a hip fracture. Men and women over the age of 60 are at higher risk of osteoporosis than younger people. Nevertheless, it is possible to have osteoporosis at a much earlier age.
Osteoporosis has no obvious symptoms, but the good news is that you can take steps to prevent it. Osteoporosis is a largely treatable disease. And with a combination of lifestyle changes and appropriate medical treatment, many fractures can be avoided.
Facts about osteoporosis include:
- Osteoporosis accounts for more days in the hospital than any other disease including breast cancer and diabetes.
- The risk of an osteoporosis fracture is up to 27% higher than the risk of getting prostate cancer.
- Approximately 80% of the people who have had at least one osteoporotic fracture are neither identified nor treated for osteoporosis. It is a silent disease.
In This Article:
- What Is Osteoporosis?
- What Causes Osteoporosis?
- What are the Symptoms of Osteoporosis?
- How is Osteoporosis Diagnosed?
- How is Osteoporosis Treated?
- Is It Possible to Prevent Osteoporosis?
- Novus Spine & Pain Center
- Osteoporosis Resources
What Is Osteoporosis?
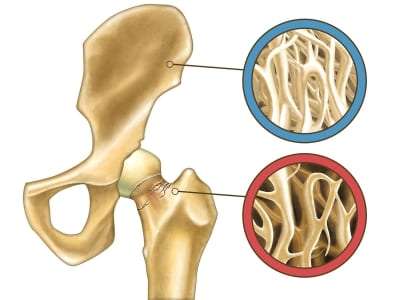
Osteoporosis, a term that literally means “porous bone,” is a disease in which the density and quality of bone are reduced. The condition causes the bones to become more porous, resulting in bones that become weak and brittle, therefore increasing the risk of fracture. This disease can result in bones becoming so brittle that a fall, or even mild stresses such as bending over or coughing, can cause a fracture. Osteoporosis-related fractures most commonly occur in the hip, wrist, and spine.
Osteoporosis is a disease of progressive bone loss. The loss of bone is silent and progressive, often without any symptoms until the first fracture occurs. Osteoporosis affects men and women of all races. However, Asian and Caucasian women who are past menopause are at the highest risk of having osteoporosis.
Fortunately, osteoporosis is largely preventable. And in patients with the disease, doctors can diagnose and treat it before it results in a broken bone. Even after a patient experiences a fracture, further problems are avoidable with proper treatment.
What Causes Osteoporosis?
Bones are living tissue and in a constant state of renewal, with new bone being made as old bone breaks down. From birth until young adulthood, the body makes new bone faster than it breaks down old bone. Most people reach their peak bone mass (most dense bones) by the early 20s. Then, as we age, we lose bone mass faster than it’s created. For people with osteoporosis, bone loss outpaces the growth of new bone, resulting in porous and brittle bones that are more prone to fracture.
The likelihood of developing osteoporosis partially depends on how much bone mass was attained during your youth. Doctors are unsure of the exact medical causes of osteoporosis, but they have identified many of the major factors that can lead to the disease:
- Aging. Everyone loses bone with age. The risk increases after the age of 50.
- Diet. Poor nutrition leads to not eating enough fruits and vegetables to supply nutrients to the body (magnesium, potassium, vitamins C and K), a lack of calcium (vitamin D), and not getting enough protein.
- Gender. Women are 4 times more likely to develop osteoporosis than men. In women, an estrogen deficiency can also cause bone loss.
- A family history of fractures; a small, slender body build; fair skin; and Caucasian or Asian ethnicity can increase the risk for osteoporosis. Doctors believe heredity may also explain why some people develop osteoporosis early in life.
- Lifestyle. Having an inactive lifestyle, and also consuming too much alcohol, sodium, or caffeine.
- Medications and some illnesses. Osteoporosis has been linked to the use of some medications, including steroids; and to other illnesses, including some thyroid problems.
- Nutrition and lifestyle. Poor nutrition, including a low calcium diet, low body weight, and a sedentary lifestyle have been linked to osteoporosis, as have smoking and excessive alcohol use.
- Smoking increases the rate of bone loss and the chance of a fracture.
What are the Symptoms of Osteoporosis?
Often the first symptom of osteoporosis is a fracture. Because bone loss is gradual and painless, there are usually no symptoms to indicate you are developing osteoporosis. This is why osteoporosis is often referred to as a silent disease. Most people don’t know they have osteoporosis until their bones become so weak that a sudden strain, bump, or fall causes a fracture.
Most commonly, a fracture due to osteoporosis occurs at the spine, the wrist, or the hip, although they can occur in other bones as well.
Spinal fractures can be difficult to diagnose. This is because they might be painless; or if there is pain, a person may not know it is caused by a fracture due to the many different causes of back pain. Collapsed vertebrae may initially be felt or seen in the form of severe back pain or spinal deformities, such as kyphosis (severely stooped posture, often called a dowager’s hump) or a loss of height.
Since there are usually no outward signs of osteoporosis, doctors will often recommend diagnostic testing, depending on the patient’s age and if there are other risk factors for the disease.
How is Osteoporosis Diagnosed?
Diagnosis of osteoporosis is usually made by a combination of a complete medical history and physical examination.
If your doctor diagnoses low bone mass, he or she may want to perform additional tests to rule out the possibility of other diseases that can cause bone loss, including osteomalacia (a metabolic bone disease characterized by abnormal mineralization of bone) or hyperparathyroidism (overactivity of the parathyroid glands).
When osteoporosis is suspected, skeletal x-rays and specialized laboratory tests may be necessary. One is a bone mineral density (BMD) test, sometimes called bone densitometry. The test is a safe, painless x-ray technique that compares bone density to the peak bone density that someone of your same sex and ethnicity should have reached at 20 to 25 years of age. Doctors often perform a bone densitometry in women at the time of menopause.
Traditional X-rays identify spine fractures, but they can’t measure bone density. Bone mineral density (BMD) has to be measured by more specialized techniques. There are several different types of BMD tests that can detect very small percentages of bone loss for assessing the risk of osteoporosis. The BMD test can determine the rate of bone loss (when conducted regularly over several years) and predict the chances of future fractures.
How is Osteoporosis Treated?
Treatment of osteoporosis is based on an estimate of the risk of breaking a bone in the next ten years, using information from the BMD test. If there is a low risk, treatment will focus on modifying risk factors for bone loss and falls, instead of medication.
Early treatment of osteoporosis can ease pain, while limiting and preventing fractures. In some cases, it is possible to stop bone loss. Because lost bone cannot be replaced, treatment for osteoporosis focuses on the prevention of further bone loss. The treatment for each patient is based upon:
- The patient’s age, gender, overall health, and medical history.
- The extent of the disease and the anticipated rate of bone loss.
- The patient’s tolerance for specific medications, procedures, and therapies.
A comprehensive osteoporosis treatment program, similar to prevention methods, includes a focus on proper nutrition, exercise, and safety issues. In addition, the doctor may prescribe medication to slow or stop bone loss, increase bone density, and reduce fracture risk.
Although exercise and nutrition therapy are often key components of a treatment plan for osteoporosis, there are other treatments as well.
Lifestyle and Home Remedies
The following suggestions may help reduce your risk of developing osteoporosis or experiencing broken bones:
- Avoid excessive alcohol. Consuming more than two alcoholic drinks a day may decrease bone formation. Being under the influence of alcohol can also increase the risk of falling.
- Don’t smoke.
- Exercise is an essential component of an osteoporosis prevention and treatment program. Exercise not only improves your bone health, but it increases muscle strength, coordination, and balance, while also leading to better overall health. Although exercise is good for someone with osteoporosis, it should not put any sudden or excessive strain on your bones. Your doctor may also recommend specific exercises to strengthen and support your back.
- Fall prevention is a serious concern for men and women with osteoporosis. Falls can increase the likelihood of fracturing a bone. Falls can be the result of impaired vision or balance, chronic diseases that affect mental or physical function, and certain medications (sedatives and antidepressants). Patients should wear low-heeled shoes with nonslip soles, and check their home for electrical cords, area rugs, and slippery surfaces that might cause a fall. Keep rooms brightly lit, install grab bars just inside and outside of shower doors, and make sure you can get into and out of your bed easily.
- Nutrition: The foods we eat contain a variety of vitamins, minerals, and other essential nutrients that help keep our bodies healthy. All of these nutrients are needed in balanced proportions. Calcium and vitamin D are necessary for strong bones and for your heart, muscles, and nerves to function properly.
Hormones
Osteoporosis is more common in people who have too much or too little of certain hormones in their body. Examples include:
- Testosterone. Men experience a gradual reduction in testosterone levels as they age. Treatments for prostate cancer that reduce testosterone levels in men are likely to accelerate bone loss in men.
- Thyroid problems. Too much thyroid hormone can cause bone loss. This can occur if your thyroid is overactive, or if you take too much thyroid hormone medication to treat an underactive thyroid.
- Other glands. Osteoporosis is associated with overactive parathyroid and adrenal glands.
- Estrogen replacement therapy (ERT) is often recommended for women at high risk for osteoporosis to prevent bone loss and reduce fracture risk. A measurement of bone density when menopause begins may help determine whether ERT is the proper treatment.
- Selective estrogen receptor modulators (SERMs). New anti-estrogens (SERMs) can increase bone mass, decrease the risk of spine fractures, and lower the risk of breast cancer.
- Calcitonin is another medication used to decrease bone loss. A nasal spray form of this medication increases bone mass, limits spine fractures, and may offer some pain relief.
- Bisphosphonates are a class of drugs that markedly increase bone mass and prevent both spine and hip fractures.
ERT, SERMs, calcitonin, and bisphosphonates all offer patients with osteoporosis an opportunity to increase bone mass and significantly reduce fracture risk. Prevention is preferable to waiting until treatment is necessary.
The FDA has also approved some injections, IV infusions, tablets, nasal sprays, and patches, which have been shown to reduce fractures in randomized studies.
Is It Possible to Prevent Osteoporosis?
Many things increase your chances of developing osteoporosis that you have no control over, such as your genes, age, and sex. However, that doesn’t mean you can’t prevent the disease.
Some risk factors for osteoporosis that are out of your control include:
- Gender. Women are much more likely to develop osteoporosis than men.
- Age. The older you are, the greater the risk of osteoporosis.
- Race. You are at the greatest risk of osteoporosis if you’re of Caucasian or Asian descent.
- Family history. Having a parent or sibling with osteoporosis puts you at higher risk of having the disease, especially if your mother or father experienced a hip fracture.
- Body frame size. Men and women who have small body frames tend to have a higher risk of osteoporosis, because they may have less bone mass to draw from as they age.
Risk factors you can change:
- Hormones. The abnormal absence of menstrual periods (amenorrhea) and low estrogen levels (menopause) in women, and low testosterone levels in men, can bring on osteoporosis.
- Eating disorders. Severely restricting food intake and being underweight (as with anorexia nervosa) weakens bones in both men and women.
- Calcium and vitamin D intake. A lifetime diet low in calcium and vitamin D makes you more prone to bone loss.
- Gastrointestinal surgery. Surgery to reduce the size of your stomach or to remove part of the intestine limits the amount of surface area available to absorb nutrients, including calcium.
- Medication use. Long-term use of certain medications, such as glucocorticoids and some anticonvulsants, can lead to loss of bone density and fractures.
- Lifestyle. An inactive lifestyle or extended bed rest tends to weaken bones.
- Cigarette smoking is bad for bones as well as the heart and lungs.
- Alcohol intake. Excessive consumption of alcohol increases the risk of bone loss and fractures.
To protect your bones, men and women of all ages should:
- Consume adequate amounts of calcium and vitamin D.
- Follow national nutritional guidelines for protein, fruit, and vegetable intakes.
- Have sufficient weight-bearing activity.
- Limit alcohol intake.
- Stop smoking.
Women who have gone through menopause or men older than age 50 should:
- Talk to a doctor about their risk of osteoporosis and related fractures.
- Follow a diet rich in fruits and vegetables that includes adequate vitamin D and calcium, with supplements prescribed as necessary.
- Do regular weight-bearing and muscle-strengthening exercises.
- Assess fall risks and consider appropriate prevention methods.
- Only drink alcohol in moderation.
- Measure their height each year.
Here are some tips to help eliminate the environmental factors that lead to falls.
Outdoors:
- Use a cane or walker for added stability.
- Wear rubber-soled shoes for traction.
- Walk on grass when sidewalks are slippery.
- In winter, sprinkle salt or kitty litter on slippery sidewalks to increase traction.
Indoors:
- Keep rooms free of clutter, especially on floors.
- Keep floor surfaces smooth but not slippery.
- Wear supportive, low-heeled shoes even at home.
- Avoid walking in socks, stockings, or slippers.
- Be sure carpets and area rugs have skid-proof backing or are tacked to the floor.
- Be sure stairwells are well lit and that stairs have handrails on both sides.
- Install grab bars on bathroom walls near the tub, shower, and toilet.
- Use a rubber bath mat in the shower or tub.
- Keep a flashlight with fresh batteries beside your bed.
- If using a step stool for hard-to-reach areas, use a sturdy one with a handrail and wide steps.
- Add ceiling fixtures to rooms lit by lamps.
- Consider purchasing a cordless phone so that you don’t have to rush to answer the phone when it rings, or so that you can call for help if you fall.
- Be careful on highly polished floors that become slick and dangerous when wet.
Do you know your personal risk factors for osteoporosis? Take the IOF (International Osteoporosis Foundation) One Minute Osteoporosis Risk Awareness Test to find out. The test lets you determine the risk factors you can and cannot change to calculate your personal risk factor. For further information about osteoporosis, please contact the National Osteoporosis Society.
Novus Spine & Pain Center
Novus Spine & Pain Center is in Lakeland, Florida, and specializes in treating the pain caused by osteoporosis. By using a comprehensive approach and cutting-edge therapies, we work together with patients to restore function and regain an active lifestyle, while minimizing the need for opiates.
For your convenience, you may schedule an appointment online, request a call back, or call our office at 863-583-4445.
Osteoporosis Resources
What is Osteoporosis (International Osteoporosis Foundation)
Diagnosing Osteoporosis (International Osteoporosis Foundation)
Osteoporosis Overview (NIH Osteoporosis and Related Bone Diseases National Resource Center)
Osteoporosis (American Academy of Orthopaedic Surgeons)
Osteoporosis (Johns Hopkins)
Who’s At Risk? (International Osteoporosis Foundation)
Osteoporosis – Symptoms and Causes (Mayo Clinic)
Osteoporosis – Diagnosis and Treatment (Mayo Clinic)
Osteoporosis Risk and Prevention (WebMD)
Osteoporosis Treatment and Care (WebMD)
Osteoporosis (MedlinePlus)
Preventing Osteoporosis (International Osteoporosis Foundation)
Osteoporosis Fast Facts (American Bone Health)
Updated: November 15, 2021

