Effectively managing pain is crucial for overall well-being, whether you are recovering from surgery or dealing with chronic pain. Pain pumps offer a targeted approach to pain relief, delivering medication directly to the source of pain and minimizing the need for systemic medications.
If you are facing or recovering from surgery, managing chronic pain, or considering different pain management options, understanding the role of pain pumps can empower you to participate in your care plan actively.
This article explores the different types of pain pumps and their applications in various surgical procedures and chronic pain conditions. We will also examine the potential benefits pain pumps offer and various applications for their use.
In This Article:
- Key Takeaways
- What is a Pain Pump?
- Benefits of Using a Pain Pump
- Potential Risks and Side Effects
- FAQs
- What is a pain pump, and how does it work?
- How long does a pain pump stay in place?
- What are the benefits of using a pain pump for pain relief?
- What are the potential risks or side effects of pain pumps?
- Can I shower with a pain pump?
- Is it safe to sleep with a pain pump?
- What medications are used in pain pumps?
- What should I do if I experience any problems with my pain pump?
- Conclusion
- Novus Spine & Pain Center
- Additional Resources
Key Takeaways
- Versatile Pain Relief: Pain pumps offer targeted pain management for various conditions, including post-surgical pain, chronic pain syndromes, and spasticity.
- Mechanism of Action: Pain pumps deliver medication directly to the pain source via a catheter, minimizing systemic side effects and providing consistent relief.
- Types of Pain Pumps: External and implantable pain pumps cater to different needs and durations of treatment.
- Benefits: Pain pumps offer improved pain control, reduced reliance on opioids, enhanced quality of life, and customizable treatment options.
- Potential Risks: Risks include infection, catheter complications, pump malfunction, and medication-specific side effects.
- Active Pain Management: Understand how pain pumps work and actively participate in your care plan to optimize pain relief and improve overall well-being.
What is a Pain Pump?
A pain pump is a method of pain control that delivers medication directly to the source of pain, whether it be a surgical site or a specific area affected by a chronic pain condition. This targeted approach offers significant advantages over traditional oral or intravenous pain medications by minimizing side effects and providing consistent pain relief.
Definition and Mechanism
A pain pump, also known as a patient-controlled analgesia (PCA) pump or an intrathecal drug delivery system, is a small device that delivers pain medication continuously through a catheter placed near the nerves responsible for transmitting pain signals.
This localized delivery minimizes the side effects of systemic pain medications circulating throughout the body. The medications used in pain pumps are typically local anesthetics, which numb the area, medicine to block pain signals, or other analgesics tailored to a specific condition.
How it Works
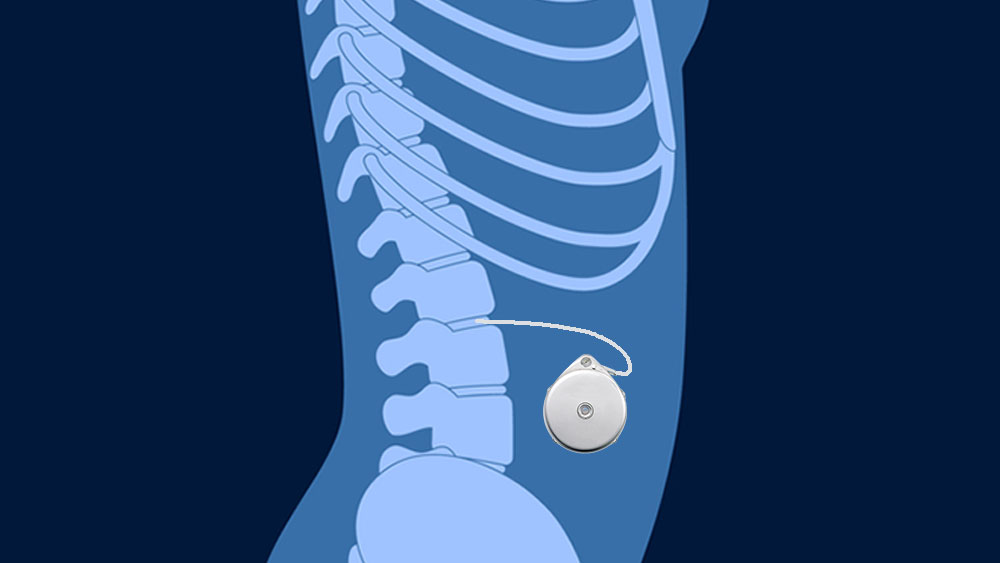
The pain pump system consists of two main components: the pump, which holds the medication, and a thin, flexible tube called a catheter. The catheter is strategically positioned near the nerves, transmitting pain signals from the affected area. The pump is attached to the catheter and either secured to the patient’s clothing or implanted.
The medication is delivered continuously to the targeted area, providing consistent pain relief. Some pain pumps also have a feature allowing patients to self-administer a small, pre-programmed dose of medication as needed by pressing a button.
Types of Pain Pumps
There are several types of pain pumps, each designed for specific applications and levels of patient control:
- External Pain Pumps: These are commonly used for post-surgical pain relief and some chronic pain conditions. They are worn externally and deliver medication through a catheter placed under the skin.
- Implantable Pain Pumps: These are surgically implanted under the skin, usually in the abdomen, and deliver medication directly to the spinal cord (intrathecal delivery). They are primarily used for chronic pain conditions that do not respond well to other treatments.
Applications
- Post-Surgical Pain Management: Pain pumps are frequently used after surgeries, including orthopedic, abdominal, and thoracic procedures.
- Chronic Pain Conditions: Pain pumps can be beneficial for managing chronic pain conditions such as complex regional pain syndrome (CRPS), failed back surgery syndrome, and cancer-related pain.
- Spasticity Management: Pain pumps can sometimes deliver medications that help reduce muscle spasticity associated with conditions like multiple sclerosis or cerebral palsy.
The choice of pain pump and catheter placement depends on the underlying condition, the type of pain, and the patient’s needs.
Benefits of Using a Pain Pump
Pain pumps offer a multifaceted approach to pain management, providing numerous advantages over traditional methods like oral or intravenous medications. These benefits extend to various applications, including post-surgical pain relief and management of chronic pain conditions.
Effective Pain Management
Pain pumps provide continuous, targeted pain relief directly to the source of pain. By consistently delivering medication, a pain pump maintains a steady level of pain relief, preventing pain from worsening and eliminating the fluctuations in pain levels that often occur with oral or intermittent medications. By maintaining stable pain control, patients are more likely to experience higher levels of comfort and satisfaction during their recovery or daily lives.
Improved Quality of Life
For individuals with chronic pain, pain pumps can significantly improve their quality of life. By reducing pain intensity and frequency, pain pumps can enable patients to engage in daily activities, work, and social interactions previously limited by pain. This can lead to greater independence, an improved mood, and better overall well-being.
Reduced Side Effects
One significant advantage of pain pumps is their ability to deliver medication directly to the source of pain. This localized approach minimizes the concentration of medication in the bloodstream, reducing the risk of systemic side effects commonly associated with oral or intravenous medications. In addition, patients using pain pumps may experience fewer side effects such as nausea, vomiting, constipation, drowsiness, and cognitive impairment.
Lower Medication Doses
Because pain pumps deliver medication directly to the affected area, lower doses are often needed compared to oral or intravenous routes. This can further minimize the risk of side effects and reduce the potential for medication interactions.
Customizable Treatment
Pain pumps offer customizable treatment options. Pain management doctors can adjust the medication dosage and delivery schedule based on individual needs and responses, allowing personalized pain management tailored to each patient’s condition and pain level.
Reduced Reliance on Opioids
For both post-surgical and chronic pain management, pain pumps can help reduce reliance on opioid medications. This is particularly important due to the potential for opioid-related side effects, tolerance, and dependence. By providing effective pain relief with alternative medications or lower opioid doses, pain pumps can contribute to safer and more sustainable pain management strategies.
Potential Risks and Side Effects
While pain pumps offer significant benefits for managing various types of pain, it’s essential to acknowledge the potential risks and side effects associated with their use. These can range from mild and easily manageable to more severe complications that require prompt medical attention.
General Risks and Side Effects
These risks can occur with both external and implantable pain pumps:
- Infection: There is a risk of infection at the catheter insertion site or, in the case of implantable pumps, at the surgical site where the pump is implanted. Proper sterile techniques during insertion and regular monitoring are key to minimizing this risk. Signs of infection include redness, swelling, pain, or discharge.
- Catheter-Related Issues: The catheter can become blocked, kinked, or dislodged, preventing medication delivery. This may require catheter repositioning or replacement. Symptoms of catheter problems include increased pain, a change in the flow of medication, or leakage from the insertion site.
- Pump Malfunction: While rare, the pump can malfunction, requiring adjustments or replacement. This might be indicated by a lack of pain relief, an alarm on the pump, or a change in the pump’s operation.
- Bleeding and Hematoma: Bleeding can occur at the catheter insertion site or pump implantation site, resulting in a hematoma (blood collection in tissue). This usually resolves on its own but may require further evaluation in some cases.
Implantable Pump-Specific Risks
- Nerve Damage: In rare instances, the catheter can cause damage to nearby nerves, leading to numbness, tingling, or weakness. This is more common with intrathecal pumps, where the catheter is placed in the spinal cord.
- Spinal Cord Injury: Although very rare, there is a risk of spinal cord injury during the implantation procedure for intrathecal pumps.
- Cerebrospinal Fluid Leak: Intrathecal pumps can cause a leak of cerebrospinal fluid, which can potentially lead to headaches, nausea, or dizziness.
Medication-Specific Risks
The specific medications used in a pain pump can also carry their own set of potential risks and side effects:
- Local Anesthetics: These can cause temporary numbness or weakness in the area surrounding the catheter. In rare cases, systemic toxicity can occur, leading to cardiac and neurological complications.
- Opioids: While effective for pain relief, opioid medications can cause a range of side effects when delivered by a pain pump. However, the side effects may be less pronounced than with oral or intravenous opioids due to the targeted delivery of the pump, but they can still occur. Some of the common side effects of opioid medication delivered by a pain pump include nausea, constipation, itching, drowsiness, and respiratory depression. The severity of these side effects can vary depending on the individual, the specific opioid used, and the dosage.
- Other Analgesics: Other medications, such as baclofen (for spasticity), can have side effects like drowsiness, dizziness, and muscle weakness. Ziconotide, another medication used for chronic pain (such as cancer), can cause neurological side effects, including confusion, hallucinations, and memory problems. Clonidine (for low blood pressure) can cause drowsiness and dry mouth. However, localized delivery of analgesic medications through a pain pump often reduces the intensity and frequency of side effects compared to oral or intravenous administration.
Minimizing Risks
To minimize risks, pain management doctors implement a comprehensive set of precautions that are designed to safeguard patient well-being.
- Careful Patient Selection: Pain pumps are not suitable for everyone. A thorough evaluation helps determine if the benefits outweigh the risks for each individual.
- Proper Technique: Strict sterile technique is used during catheter insertion and pump implantation to reduce infection risk.
- Monitoring: Patients are closely monitored for any signs of complications.
- Patient Education: Patients receive detailed instructions on how to care for their pain pump, recognize potential problems, and when to contact their pain specialist.
Before deciding, patients must discuss the potential risks and benefits of pain pumps and different pain medications with their pain medicine physician. By understanding possible complications and working closely with their pain doctor, patients can minimize risks and optimize their pain management experience.
FAQs
What is a pain pump, and how does it work?
A pain pump is a medical device that delivers medication directly to the source of pain, providing targeted and continuous relief. It consists of a small, portable pump that holds the medication and a thin, flexible tube (catheter) that delivers the medication to the affected area. This method is used for various applications, including post-surgical pain management, chronic pain conditions like complex regional pain syndrome (CRPS), failed back surgery syndrome, and spasticity management in conditions like multiple sclerosis.
The pump can be worn externally, secured to the patient’s clothing, or implanted for long-term pain management. The catheter is strategically positioned near the nerves that transmit pain signals, allowing the medication to block pain receptors or interrupt pain signals effectively.
Some pain pumps also offer patient-controlled analgesia (PCA), enabling patients to self-administer a pre-measured dose of medication as needed. The medications used in pain pumps vary depending on the type of pain and individual needs but may include local anesthetics, opioids, or other analgesics.
How long does a pain pump stay in place?
The duration a pain pump remains in place varies significantly depending on several factors, including the type of pain pump, the underlying condition being treated, the type of medication used, and the individual patient’s needs and response to treatment.
For post-surgical pain relief, external pain pumps are typically used for a short period, ranging from 2 to 5 days. However, they may remain in place longer in cases of major surgery or complex pain management needs.
For chronic pain conditions, external pumps may be used for extended periods, or an implantable pump may be considered. With periodic medication refills, implantable pumps can remain in place for several years. The pain management physician decides whether to remove or refill a pain pump based on factors such as pain level, functional improvement, and any complications.
What are the benefits of using a pain pump for pain relief?
Pain pumps offer numerous advantages over other pain relief methods, making them valuable for various applications, including treating chronic pain conditions and post-surgical pain management. The key benefits include:
- Targeted Pain Relief: Pain pumps deliver medication directly to the source of pain, providing targeted relief for chronic conditions and post-surgical pain management. This localized approach reduces the need for systemic pain medications, minimizing side effects like nausea, drowsiness, and cognitive impairment.
- Consistent Pain Control: Pain pumps provide a continuous flow of medication, ensuring steady pain relief and preventing pain fluctuations. This leads to improved comfort and better pain management, especially for chronic pain sufferers.
- Reduced Opioid Use: Pain pumps can often achieve effective pain control with lower doses of opioids or alternative medications, reducing the risk of opioid-related side effects and dependence.
- Improved Quality of Life: Pain pumps can help patients regain function, participate in daily activities, and experience a better overall quality of life by minimizing pain. This is particularly significant for individuals with chronic pain conditions.
- Customizable Treatment: Pain pumps offer flexibility in medication choice and dosage adjustments, allowing for personalized pain management tailored to individual needs.
Overall, pain pumps provide a targeted, effective, and customizable approach to pain relief, offering potential benefits for various patient populations.
What are the potential risks or side effects of pain pumps?
While generally safe and effective, pain pumps carry potential risks and side effects that patients should be aware of. Some common side effects include nausea, vomiting, itching, and urinary retention. These are often manageable with medications or other interventions.
More serious complications, though rare, can include infection at the catheter insertion site, catheter blockage, nerve damage, and hematoma formation. Proper hygiene at the insertion site is essential. Report any signs of infection, such as redness, swelling, or discharge, to your doctor immediately. Additionally, the medications used in pain pumps can have their own set of side effects. For example, opioids carry the risk of respiratory depression and constipation, while local anesthetics can cause temporary numbness or weakness.
Can I shower with a pain pump?
Whether or not you can shower with a pain pump depends on your specific type of pump and your pain doctor’s recommendations. Some pain pumps have waterproof coverings that allow showering without disconnecting or covering the pump. However, other types of pain pumps may not be waterproof and require precautions to keep the pump dry during showering.
It’s crucial to follow the showering guidelines for your specific pain pump. If necessary, your pain management doctor will guide you on how to protect the pump and ensure that showering does not compromise the pump’s functionality or increase the risk of infection at the catheter insertion site.
Is it safe to sleep with a pain pump?
It is safe to sleep with a pain pump. External pain pumps are designed to be worn comfortably and securely, even during sleep. These external pumps are typically secured to clothing or a belt, and the catheter is taped to the skin to prevent accidental dislodgement.
However, it is essential to follow your pain physician’s instructions regarding positioning and movement while sleeping. You may be advised to avoid sleeping on the side where the catheter is inserted or to avoid excessive movement that could disrupt the pump or dislodge the catheter.
Internal (implanted) pain pumps are placed under the skin, usually in the abdomen, so they cannot be easily dislodged while sleeping. Additionally, implanted pumps are designed to be durable and withstand daily activities, including sleeping. Most patients find their implanted pumps are comfortable and do not interfere with sleep.
What medications are used in pain pumps?
The medications used in pain pumps vary depending on the type of pain being managed, the location of the pain, and individual patient needs. For both chronic pain management and post-surgical, common medications include:
- Local Anesthetics: Medications, such as bupivacaine or ropivacaine, numb the nerves in the targeted area, providing effective pain relief. They are often used for both localized chronic pain conditions and post-surgical pain.
- Opioids: Often used for moderate to severe pain, opioids require careful monitoring due to potential side effects and the risk of dependence. Morphine, hydromorphone, and fentanyl are potent opioid pain relievers that block pain signals in the brain.
- Non-steroidal Anti-inflammatory Drugs (NSAIDs): Sometimes used in combination with other medications or as an alternative to opioids, NSAIDs like ketorolac can help reduce inflammation and pain.
For other applications, such as managing spasticity, different medications may be used:
- Baclofen: A muscle relaxant commonly used to reduce spasticity associated with multiple sclerosis or spinal cord injury.
- Ziconotide: A medication used for severe chronic pain, particularly in cases where opioids are ineffective or not tolerated.
Your pain physician will determine the specific medication and dosage used in a pain pump based on a thorough assessment of your needs and medical history.
What should I do if I experience any problems with my pain pump?
If you experience any problems with your pain pump, it is important to report them immediately. This includes issues such as:
- Increased Pain or Inadequate Pain Relief: If your pain is not well-managed despite using the pain pump, you may need a dosage adjustment or a different medication.
- Signs of Infection: Redness, swelling, warmth, pain, or drainage at the catheter insertion site could indicate an infection.
- Pump Malfunction: If the pump is making unusual noises, leaking, or not delivering medication properly, it may need to be replaced.
- Other Side Effects: Excessive nausea, vomiting, difficulty urinating, or any other concerning symptoms should be reported promptly.
Your pain management specialist is best equipped to assess the situation and provide appropriate solutions. They may need to adjust the pump settings, refill the medication, or, in some cases, remove the pump and explore alternative pain management options.
Conclusion
Pain pumps are versatile pain management tools. They deliver medication directly to the source of pain for both chronic and surgical pain management. This targeted approach offers improved pain control, reduced side effects, and enhanced recovery. Pain pumps can also help manage spasticity.
While effective, pain pumps have potential risks, including infection and catheter problems. Choosing a pain pump requires careful consideration and discussion with a pain doctor. When used appropriately, pain pumps empower patients to manage their pain and improve their quality of life actively.
Novus Spine & Pain Center
Novus Spine & Pain Center is in Lakeland, Florida, and treats patients with chronic pain with numerous therapies, including pain pumps. By using a comprehensive approach and cutting-edge therapies, we work together with patients to restore function and regain an active lifestyle while minimizing the need for opiates.
For your convenience, you may schedule an appointment online, request a call back, or call our office at 863-583-4445.
Additional Resources
Intrathecal Pain Pump (Johns Hopkins)
Pain pump, Intrathecal drug pumps (Mayfield Clinic)
About Your Intrathecal Pump (Memorial Sloan Kettering Cancer Center)

