Minimally invasive kyphoplasty and sacroplasty procedures can effectively treat vertebral compression fractures (VCFs) and sacral fractures, which involve a break or crack in the sacrum, the large triangular bone at the base of the spine. These innovative procedures utilize bone cement to stabilize and strengthen the affected vertebrae, providing significant pain relief and restoring function.
VCFs can significantly impact your quality of life, causing debilitating pain, limited mobility, and even spinal deformity. These fractures, often caused by osteoporosis or trauma, result in the collapse of vertebrae, leading to a range of physical and emotional challenges.
This article explores the details of kyphoplasty and sacroplasty procedures, their benefits, risks, and the recovery process.
In This Article:
- Key Takeaways
- Kyphoplasty: Targeting Vertebral Compression Fractures
- Sacroplasty: Addressing Sacral Fractures
- Recovery and Rehabilitation
- Choosing the Right Procedure
- FAQs
- What are kyphoplasty and sacroplasty?
- Who is a good candidate for these procedures?
- How long do the procedures take?
- What is the recovery time?
- How effective are kyphoplasty and sacroplasty?
- Are there any alternatives to these procedures?
- How long do the results last?
- Conclusion
- Novus Spine & Pain Center
- Additional Resources
Key Takeaways
- Kyphoplasty and Sacroplasty: Minimally invasive procedures to treat vertebral compression fractures and sacral fractures, offering pain relief and improved function.
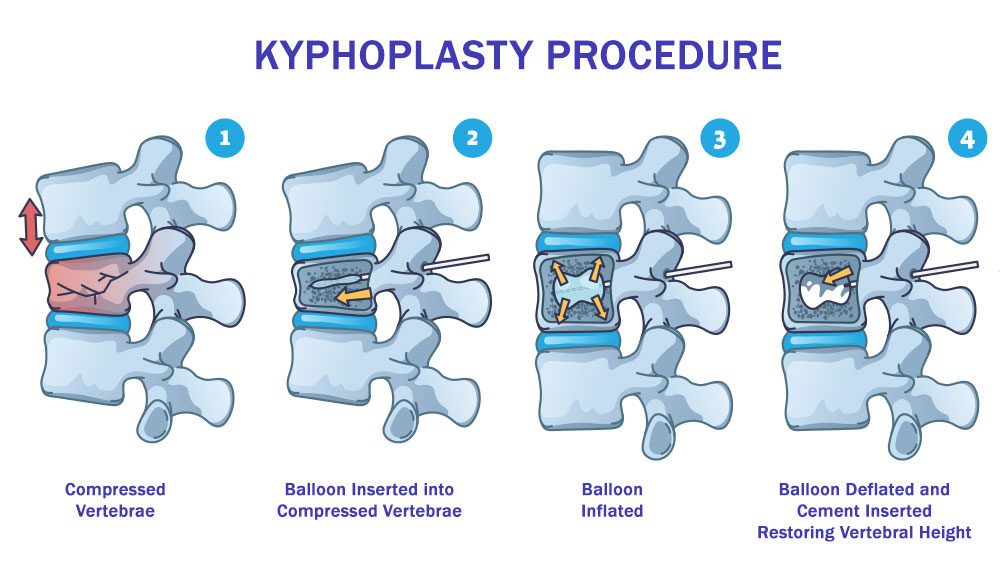
- Kyphoplasty Procedure: Involves inserting a balloon into the collapsed vertebra, restoring height and injecting bone cement for stability.
- Sacroplasty Procedure: Involves injecting bone cement directly into the fractured sacrum for pain relief and support.
- Benefits: Significant pain reduction, improved mobility, faster recovery, minimally invasive nature.
- Potential Risks: Rare complications include cement leakage, infection, and allergic reactions.
- Recovery and Rehabilitation: Essential for regaining strength, flexibility, and independence after the procedure.
- Effective and Long-Lasting Results: Both procedures provide significant pain relief and functional improvement, offering a promising solution for individuals with these fractures.
Kyphoplasty: Targeting Vertebral Compression Fractures
Kyphoplasty is a minimally invasive procedure specifically designed to address the pain and instability caused by vertebral compression fractures (VCFs). This innovative technique focuses on restoring the height and strength of collapsed vertebrae, leading to significant pain relief and improved quality of life.
Kyphoplasty Procedure
The kyphoplasty procedure is typically performed under local anesthesia and involves a few key steps:
- Needle Insertion: A thin needle is inserted into the affected vertebra under X-ray guidance.
- Balloon Inflation: A small balloon is carefully inflated within the vertebra, creating space and helping to restore its original height.
- Bone Cement Injection: Once the desired height is achieved, the balloon is deflated, and bone cement is injected into the created cavity. This cement hardens quickly, providing immediate stability and support to the vertebra.
The entire procedure usually takes less than an hour per vertebra, and patients often experience immediate pain relief.
Candidates for Kyphoplasty
Kyphoplasty is particularly beneficial for individuals with:
- VCFs Due to Osteoporosis: Osteoporosis weakens the bones, making them more susceptible to fractures, especially in the spine.
- Painful Vertebral Fractures: Kyphoplasty can effectively alleviate the pain associated with VCFs, improving mobility and function.
- Your pain doctor, a specialist in managing pain related to vertebral and sacral fractures, will assess your overall health and specific condition to determine your suitability for kyphoplasty.
Benefits and Potential Risks
Kyphoplasty offers several advantages, including:
- Reduced Pain and Improved Mobility: The procedure can significantly reduce pain and restore spinal function, allowing for greater independence and a better quality of life.
- Minimally Invasive Nature: Kyphoplasty involves small incisions and minimal tissue disruption, resulting in a faster recovery than traditional open surgery.
- Immediate Pain Relief: Many patients experience significant pain reduction immediately after the procedure.
While generally safe, kyphoplasty carries some potential risks, such as:
- Cement Leakage: In rare cases, the bone cement may leak outside the vertebra, potentially causing nerve compression or other complications.
- Infection: Although uncommon, infection can occur at the injection site.
- Allergic Reactions: Some individuals may experience allergic reactions to the bone cement or other materials used during the procedure.
It’s crucial to discuss these potential risks and benefits with your pain doctor. Their guidance and support will help you make an informed decision about kyphoplasty.
Sacroplasty: Addressing Sacral Fractures
Sacroplasty is a minimally invasive procedure designed to treat painful sacral fractures in the triangular bone at the base of the spine. Similar to kyphoplasty, this technique utilizes bone cement to stabilize the fracture, ease pain, and improve overall function.
Sacroplasty Procedure
The sacroplasty procedure is typically performed under local anesthesia and involves the following steps:
- Needle Insertion: A thin needle is carefully guided into the sacrum under X-ray visualization.
- Bone Cement Injection: Once the needle is in the correct position, bone cement is injected into the fractured area. The cement fills the cracks and voids within the bone, providing immediate stability and support.
The procedure usually takes about an hour, and patients often experience significant pain relief shortly after.
Candidates for Sacroplasty
Sacroplasty is particularly beneficial for individuals with:
- Painful Sacral Fractures: The procedure can effectively alleviate the pain associated with sacral fractures, improving mobility and quality of life.
- Osteoporosis-Related Fractures: Osteoporosis weakens the bones, increasing the risk of fractures, including those in the sacrum. Sacroplasty can be an effective treatment option for these fractures.
- Other Considerations: Your doctor will evaluate your overall health, the severity of your fracture, and other factors to determine if you’re a suitable candidate for sacroplasty.
Benefits and Potential Risks
Sacroplasty offers several advantages, including:
- Pain relief and Improved Function: The procedure can significantly reduce pain and restore function in the sacrum, allowing for greater mobility and independence.
- Minimally Invasive Procedure: Sacroplasty involves small incisions and minimal tissue disruption, resulting in faster recovery than open surgery.
- Quick Pain Relief: Many patients experience significant pain reduction soon after the procedure.
While generally safe, sacroplasty carries some potential risks, such as:
- Cement Leakage: In rare cases, the bone cement may leak outside the sacrum, potentially causing nerve compression or other complications.
- Infection: Although uncommon, infection can occur at the injection site.
- Allergic Reactions: Some individuals may experience allergic reactions to the bone cement or other materials used during the procedure.
Discussing these potential risks and benefits with your pain doctor to make an informed decision about sacroplasty is essential.
Recovery and Rehabilitation
While both kyphoplasty and sacroplasty are minimally invasive procedures, a smooth recovery and rehabilitation process is essential for optimal results and long-term well-being. Following post-procedure care and rehabilitation guidelines can help you regain strength, mobility, and independence.
Post-Procedure Care
After undergoing kyphoplasty or sacroplasty, you can expect:
- Hospital Stay and Discharge: In most cases, you can go home the same day or the following day after the procedure. Your pain doctor will provide specific instructions regarding discharge and follow-up appointments.
- Activity Restrictions and Precautions: You may need to limit certain activities, such as bending, lifting heavy objects, or driving, for a specific period. Following these recommendations is crucial to avoid complications and ensure proper healing.
- Pain Management: While many patients experience immediate pain relief, you may still feel discomfort during the initial recovery period. Your pain doctor will prescribe appropriate pain medications and provide guidance on managing any residual pain.
Rehabilitation and Physical Therapy
Rehabilitation plays a vital role in regaining strength, flexibility, and mobility after kyphoplasty or sacroplasty. Your doctor may recommend:
- Strengthening and Mobility Exercises: A physical therapist can design a personalized exercise program to help you strengthen the muscles supporting your spine and improve your range of motion.
- Fall Prevention Strategies: As osteoporosis can increase the risk of falls, your therapist may teach you techniques to improve balance and reduce fall risk.
- Regaining Independence: Rehabilitation focuses on helping you regain your independence and perform daily activities with ease and confidence.
By actively participating in your rehabilitation program and following your doctor’s instructions, you can optimize your recovery and enjoy a better quality of life after kyphoplasty or sacroplasty.
Choosing the Right Procedure
While both kyphoplasty and sacroplasty offer effective solutions for vertebral and sacral fractures, selecting the appropriate procedure depends on various factors specific to your condition and overall health. Understanding these factors and consulting with your pain doctor will help you make an informed decision and achieve the best possible outcome.
Factors to Consider
Several key factors influence the choice between kyphoplasty and sacroplasty:
- Fracture Location: Kyphoplasty is designed for vertebral compression fractures, while sacroplasty addresses fractures in the sacrum.
- Severity of Pain and Disability: The level of pain and functional impairment you’re experiencing will play a role in determining the most suitable procedure.
- Overall Health and Medical History: Your general health, any underlying medical conditions, and previous treatments are all carefully considered when your pain doctor recommends a treatment plan.
- Bone Quality: The strength and density of your bones, especially in the context of osteoporosis, can impact the effectiveness of each procedure.
Consulting with Your Pain Doctor
Open communication with your pain doctor is crucial when choosing between kyphoplasty and sacroplasty. During your consultation, be prepared to:
- Discuss Your Symptoms and Concerns: Explain the pain you’re experiencing, any limitations in mobility, and how the fracture affects your daily life.
- Review Your Medical History: Provide your pain doctor with a comprehensive overview of your medical history, including any previous fractures, surgeries, or chronic conditions.
- Ask Questions About Each Procedure: Seek clarification on the specifics of kyphoplasty and sacroplasty, including the potential risks, benefits, and recovery process for each.
- Understand the Expected Outcomes: Discuss your goals for treatment and what you can realistically expect in terms of pain relief, improved function, and recovery time.
By actively participating in the decision-making process and working closely with your pain doctor, you can choose the procedure that best suits your specific needs and a successful recovery.
FAQs
What are kyphoplasty and sacroplasty?
Kyphoplasty and sacroplasty are minimally invasive procedures used to treat painful fractures in the spine. Kyphoplasty specifically targets vertebral compression fractures, which often occur in the thoracic and lumbar spine due to osteoporosis or trauma. These fractures can cause significant pain, limited mobility, and even spinal deformity. During kyphoplasty, a balloon is inserted into the collapsed vertebra to restore its height, and then bone cement is injected to stabilize the bone.
Sacroplasty, on the other hand, addresses fractures in the sacrum, the triangular bone at the base of the spine. These fractures can also cause significant pain and disability. In sacroplasty, bone cement is injected directly into the fractured sacrum to provide stability and pain relief. Both procedures are typically performed under local anesthesia and offer a quicker recovery compared to traditional open surgery.
Who is a good candidate for these procedures?
Kyphoplasty and sacroplasty are typically recommended for individuals experiencing pain and limited mobility due to vertebral compression fractures (VCFs) or sacral fractures. These fractures often occur as a result of osteoporosis, a condition that weakens the bones, making them more susceptible to breakage. Additionally, trauma or injury can also lead to these types of fractures.
Ideal candidates for these procedures are those who have not found relief through conservative treatments like pain medications, physical therapy, or wearing a brace. It’s important to consult with your pain doctor to determine if you’re a suitable candidate, as they will assess your overall health, the severity of your fracture, and any underlying medical conditions that may influence the decision.
How long do the procedures take?
The duration of kyphoplasty and sacroplasty can vary depending on the number of vertebrae or sacral fractures being treated. However, on average, each procedure typically takes about an hour to complete.
For instance, if a patient has two vertebral compression fractures requiring kyphoplasty, the entire procedure may take around two hours. Similarly, treating a sacral fracture with sacroplasty will likely take approximately one hour. It’s important to note that these are estimates, and the actual duration will vary depending on individual circumstances and the complexity of the case.
What is the recovery time?
Both kyphoplasty and sacroplasty are minimally invasive procedures, which generally translate to shorter recovery times than traditional open surgery. In most cases, patients can go home the same day or the day after the procedure.
While the initial recovery period may involve some activity restrictions and mild discomfort, many individuals experience significant pain relief and improved mobility within a few days. Full recovery typically takes a few weeks, during which physical therapy may be recommended to regain strength and flexibility. It’s crucial to follow all post-procedure instructions and attend any follow-up appointments to ensure a smooth and successful recovery.
How effective are kyphoplasty and sacroplasty?
Both kyphoplasty and sacroplasty have proven highly effective in treating their specific fractures. Studies and clinical experience show that these procedures significantly reduce pain and improve mobility in a majority of patients. The immediate stabilization the bone cement provides often leads to rapid pain relief, allowing individuals to regain their independence and engage in daily activities more comfortably.
Furthermore, these procedures can also help prevent further vertebral collapse and spinal deformity, preserving spinal function and overall quality of life. While individual results may vary, kyphoplasty and sacroplasty are generally considered safe and effective treatment options for vertebral compression fractures and sacral fractures, respectively.
Are there any alternatives to these procedures?
Alternative treatment options are available for vertebral compression fractures (VCFs) and sacral fractures, depending on the severity of the fracture and the patient’s overall health. Initially, conservative approaches like medication for pain, physical therapy to enhance strength and mobility, and spinal bracing are commonly suggested.
In some cases, vertebroplasty, a similar procedure to kyphoplasty but without the balloon inflation step, may be considered. For more complex or severe fractures, traditional open surgery might be necessary, although this is less common due to the advancements in minimally invasive techniques like kyphoplasty and sacroplasty. It’s essential to discuss all available options with your pain doctor to determine the most appropriate treatment plan for your individual needs and circumstances.
How long do the results last?
Both kyphoplasty and sacroplasty can provide long-term pain relief and functional improvement. The injected bone cement creates a stable internal cast within the fractured bone, restoring its strength and preventing further collapse. In most cases, patients experience lasting benefits from these procedures, with reduced pain and improved mobility for many years.
However, it’s essential to remember that these procedures do not cure the underlying cause of the fractures, such as osteoporosis. Therefore, addressing any underlying conditions and taking preventive measures to reduce the risk of future fractures is crucial. This may include medications, lifestyle changes, and ongoing follow-up care with your doctor.
Conclusion
Kyphoplasty and sacroplasty have revolutionized the treatment of vertebral compression fractures and sacral fractures, offering a minimally invasive path to pain relief, improved mobility, and enhanced quality of life. These procedures empower individuals to overcome the limitations imposed by these debilitating conditions and reclaim their independence.
If you’re struggling with the pain and limitations of vertebral compression fractures or sacral fractures, don’t hesitate to consult with a qualified pain doctor. They can assess your condition, discuss your treatment options, and help you determine whether kyphoplasty or sacroplasty is the right choice. You don’t have to live with the burden of chronic pain and limited mobility.
Novus Spine & Pain Center
Novus Spine & Pain Center is in Lakeland, Florida, and treats patients with chronic pain with numerous therapies, including kyphoplasty and sacroplasty. By using a comprehensive approach and cutting-edge therapies, we work together with patients to restore function and regain an active lifestyle while minimizing the need for opiates.
For your convenience, you may schedule an appointment online, request a call back, or call our office at 863-583-4445.
Additional Resources
Kyphoplasty (Cleveland Clinic)
Kyphoplasty (Johns Hopkins Medicine)
Kyphoplasty Procedure Overview (Spine-health)
Sacroplasty (UCLA Health)

