 Venous ulcers are open skin sores that can affect any area of the body but most often occur on the legs. It is estimated that about 1% of Americans have venous ulcers. They’re more common in older people, particularly women, and more likely to occur with people who have varicose veins. Other types of people who have an increased chance of getting a venous ulcer include:
Venous ulcers are open skin sores that can affect any area of the body but most often occur on the legs. It is estimated that about 1% of Americans have venous ulcers. They’re more common in older people, particularly women, and more likely to occur with people who have varicose veins. Other types of people who have an increased chance of getting a venous ulcer include:
- Those who have suffered previous leg injuries.
- Those who smoke.
- Those who are overweight or obese.
- Anyone with a circulation problem, such as blood clots or phlebitis (inflammation of a vein that may result in painful swelling).
Venous ulcers are sometimes called venous insufficiency ulcers, stasis leg ulcers, and venous leg ulcers.
In This Article:
- What Are Venous Ulcers?
- What Causes Venous Ulcers?
- What are the Symptoms of Venous Ulcers?
- How are Venous Ulcers Diagnosed?
- How are Venous Ulcers Treated?
- Is It Possible to Prevent Venous Ulcers?
- Novus Spine & Pain Center
- Venous Ulcers Resources
What Are Venous Ulcers?
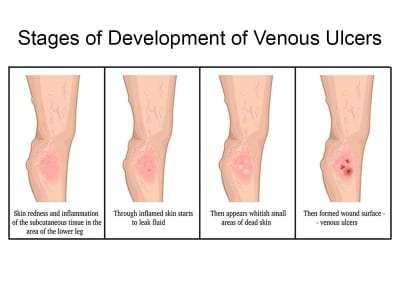
A venous skin ulcer is a sore on the leg that heals slowly, usually because of blood flow (circulation) problems in the leg veins. When leg veins do not push blood back up to the heart as they should, the blood backs up (pools), creating extra pressure in the veins. If the condition is not treated, the increased pressure and excess fluid in the affected area can cause an open sore to form.
Because of the continuous pressure, venous ulcers can linger anywhere from a few weeks to years and lead to more serious problems if untreated. Most venous ulcers occur on the lower leg, above the ankle.
What Causes Venous Ulcers?
Any condition that causes blood to pool in the veins of the leg is a potential cause of venous ulcers, including venous insufficiency, varicose veins, deep vein thrombosis, and heart failure.
The increased blood pressure created by pooling blood in the leg prevents nutrients and oxygen from getting to tissues, causing cells to die, damaging the tissue, and an ulcer (wound) can form that may or may not be painful.
Other medical conditions that can cause venous ulcers include:
- Poor circulation, often caused by arteriosclerosis.
- Other blood clotting disorders and circulation that may or may not be related to atherosclerosis.
- Diabetes.
- Renal (kidney) failure.
- Hypertension (treated or untreated).
- Lymphedema (swelling that results from impaired flow of the lymphatic system).
- Inflammatory diseases (vasculitis, lupus, scleroderma, and other rheumatological conditions).
- Other medical conditions such as high cholesterol, heart disease, high blood pressure, sickle cell anemia, and bowel disorders.
- History of smoking (either current or past).
- Pressure caused by lying in one position too long.
- Genetics (ulcers may be hereditary).
- A malignancy (tumor or cancerous mass).
- Infections.
- Certain medications.
What are the Symptoms of Venous Ulcers?
Venous ulcers are sores in the skin (usually the inside of the leg just above the ankle) that most often result from weak blood circulation. Therefore, stasis dermatitis and venous insufficiency are commonly associated with venous ulcers.
A patient suffering from a venous ulcer will usually experience a swollen leg, often accompanied by a burning feeling around the sore. Signs and symptoms of venous ulcers include:
- The leg has a feeling of heaviness and cramping.
- The area of the venous ulcer turns a dark red, purple, or brown, and there is hardened skin (a sign of blood pooling).
- The sore is shallow with a red base, sometimes covered by yellow tissue.
- The venous ulcer has unevenly shaped borders.
- The skin surrounding the sore may be shiny, tight, warm, or hot.
- If the sore becomes infected, it may have a bad odor, and pus may drain from the wound.
- There is general leg pain.
A typical complication associated with venous ulcers is an infection of the affected tissue. Typically, the ulcer itself is relatively painless. Any pain that occurs is a result of an infection or from swelling (edema). In some cases, the entire leg will become swollen, making the skin more firm and reddish-brown in color.
How Are Venous Ulcers Diagnosed?
For a leg wound that isn’t healing or may be infected, the doctor will do a visual examination of the sore and the surrounding skin to determine if it is a venous ulcer. The doctor will also evaluate the patient’s medical history to determine if there is a history of ongoing (chronic) conditions, such as diabetes or hardening of the arteries.
In some cases, the doctor may also perform tests such as X-rays or a CT scan to check the veins and the area around the ulcer in more detail.
In some cases, an MRI and noninvasive vascular studies may be ordered to help develop a treatment plan. Other tests include:
- Ankle-Brachial Index (ABI). A test to compare the blood pressure measured at the ankle with the blood pressure measured at the arm to determine if there is also arterial insufficiency.
- Doppler ultrasonography. A noninvasive test estimates blood flow by bouncing high-frequency sound waves (ultrasound) off circulating red blood cells. (A regular ultrasound uses sound waves to produce images but cannot show blood flow.)
- Venography. Using X-rays with an intravenous (IV) contrast dye to visualize the veins. The dye causes the blood vessels to appear opaque on the X-ray image, allowing the doctor to see the blood vessels. This is one of the more accurate tests to diagnose deep vein thrombosis (DVT) and other abnormalities.
Sometimes, an ulcer can lead to serious skin and bone infections. In rare cases, a venous ulcer can lead to skin cancer.
How Are Venous Ulcers Treated?
Venous ulcers need proper care and treatment to prevent infection and to heal. The Lakeland pain management doctors at the Vein Clinic work with each patient to determine the cause of the ulcer and develop an individualized treatment plan. The treatment goals are to relieve pain, speed recovery, and heal the wound. Treatment may include focusing on the circulatory or vein problems causing the ulcers.
The most common treatment to reduce the swelling is a compression bandage or stocking, which can help improve blood circulation in the legs, boosting the body’s ability to heal the sore. Some compression bandages may require the patient to wear them continuously, with a doctor replacing them every few days. Others are worn only during the day, with the patient putting them on and removing them.
In treating venous ulcers, it is essential to keep the site infection-free. Special medication may be applied under the bandages or stockings to help during the healing process.
If a venous ulcer becomes infected by bacteria, the doctor may prescribe antibiotics to kill the infection. A moist dressing may be used to help the ulcer heal more quickly.
Other treatment options for home care include:
- Apply a dressing to the ulcer and change as directed.
- Apply an antibacterial ointment or another topical medicine to prevent or treat an infection.
- Avoid products that cause skin sensitivity.
- Clean the wound regularly.
- Keeping the wound clean and dry.
- Put your feet above your heart as often as possible to help circulation. Typically, a half-hour at a time, 3 or 4 times a day. For example, lie down with feet elevated on pillows.
- Take a walk or exercise every day. Regular activity helps improve blood flow.
- Take oral antibiotic medicines to prevent or treat an infection.
- Wear appropriate shoes.
- Drink plenty of fluids.
- Follow a healthy diet that includes plenty of fruits and vegetables.
If the ulcers do not heal, surgery may be necessary to improve blood circulation. If surgery is necessary, the doctor may recommend subfascial endoscopic perforator surgery. This minimally-invasive procedure uses an endoscope (a small, flexible tube with a light) to clip and tie off the perforator veins in the calf. Doing so allows blood to drain into healthy veins and improves ulcer healing.
Most venous ulcers heal after 3 or 4 months of treatment. However, some can take longer or require a skin graft to close up the opening in the skin. Some may never clear up completely.
Is It Possible to Prevent Venous Ulcers?
The first step in preventing venous ulcers is preventing vein problems. Healthy habits are essential to help maintain proper blood flow in the legs. There are various ways to help prevent venous ulcers through lifestyle changes, diet, and medication. The Lakeland vein clinic pain management doctors recommend:
- Quit smoking. Smoking is bad for blood vessels and contributes to blood clotting in the veins.
- Lose weight if you’re overweight or obese.
- Maintain an ideal weight.
- Exercise as much as possible. Moving and staying active helps with blood flow. Check with your doctor about starting a walking program.
- Eat healthy foods and get plenty of sleep at night.
- Reduce the amount of salt in your diet.
- Control your blood cholesterol and triglyceride levels by making dietary changes and taking the medications your doctor prescribes.
- If you have diabetes, keep your blood sugar level under control to help you heal faster.
- Manage blood pressure and cholesterol levels.
- Talk to your doctor about taking aspirin to prevent blood clots.
- Avoid crossing legs while sitting.
- Avoid extreme temperatures.
- Avoid sitting or standing for extended periods of time.
- Avoid tight-fitting clothing and ensure that footwear is fitted correctly to avoid points of rubbing or pressure.
- Examine feet (especially between the toes) and legs daily for any unusual changes in color or the development of sores.
- Protect legs and feet from injury and infection.
- Raise (elevate) your legs for a short time, especially if you stand for extended periods.
Wearing compression stockings can also help. They can:
- Prevent blood from pooling in your legs.
- Help you avoid significant swelling.
- Reduce your risk for venous ulcers.
Novus Spine & Pain Center
Novus Spine & Pain Center is in Lakeland, Florida, and specializes in treating venous ulcers. By using a comprehensive approach and cutting-edge therapies, we work together with patients to restore function and regain an active lifestyle, while minimizing the need for opiates.
For your convenience, you may schedule an appointment online, request a call back, or call our office at 863-583-4445.
Venous Ulcers Resources
More information about Venous Ulcers is available from:
American Venous Forum
2800 West Higgins Road, Suite 440
Hoffman Estates, IL 60169
Tel: 727.350.1580
Email: [email protected]
Society for Vascular Surgery
633 N. Saint Clair St., 22nd Floor
Chicago, IL 60611
Telephone: 312-334-2300 / 800-258-7188
Email: [email protected]
What Is a Venous Skin Ulcer (WebMD)
Venous Ulcers (Johns Hopkins)
Subfascial Endoscopic Perforator Surgery (Stanford Health Care)
Venous Ulcers – Self-Care (MedlinePlus)
Venous Leg Ulcers (American Family Physician)
Venous Insufficiency Ulcers (Wound Source)
Leg and Foot Ulcers (Cleveland Clinic)
Ankle-brachial index (Mayo Clinic)
Doppler ultrasound: What is it used for? (Mayo Clinic)
Lymphedema (MedicineNet)
Updated: April 2, 2021

