 Plantar fasciitis involves inflammation of the plantar fascia, which is a fibrous tissue that provides support to the arch of the foot. With overuse, the plantar fascia loses some of its normal elasticity, which can result in the painful condition called plantar fasciitis.
Plantar fasciitis involves inflammation of the plantar fascia, which is a fibrous tissue that provides support to the arch of the foot. With overuse, the plantar fascia loses some of its normal elasticity, which can result in the painful condition called plantar fasciitis.
What Is Plantar Fasciitis?
Plantar fasciitis is the most common cause of heel pain. Like carpal tunnel syndrome or tennis elbow, plantar fasciitis is a foot injury of the plantar fascia, a bowstring-like tissue that stretches from the heel of the foot to the toes.
When the plantar fascia becomes weak from a strain, it swells (inflammation) making the heel or bottom of the foot hurt when standing or walking.
The main symptom of plantar fasciitis is heel pain, which can occur in one foot or both feet.
Plantar fasciitis typically starts gradually with mild pain at the heel bone, sometimes called a stone bruise. Symptoms are more likely to occur after (not during) exercise. Plantar fasciitis commonly causes stabbing pain that classically occurs right after getting up in the morning, or after a period of sitting. The pain typically decreases with movement but can return after long periods of standing or sitting.
Plantar fasciitis is more common among people who are active in sports, such as running, dancing, or jumping. Although overuse is the primary cause of the injury, the likelihood of developing the condition can increase in people with tight calf muscles that limit how far their ankles can flex. Also, people with very flat feet, high arches, who are overweight, or wear shoes with inadequate support have a greater risk of developing plantar fasciitis.
Most middle-aged people (40-60 years of age) are more likely to get the condition; however, it can also occur in younger people who are on their feet a lot. Less commonly, plantar fasciitis can develop in association with other medical conditions, or underlying diseases, that cause arthritis (inflammation of the joints).
What Causes Plantar Fasciitis?
The exact cause of plantar fasciitis is not well understood. During normal walking, the plantar fascia stretches as the foot strikes the ground. Under normal circumstances, the plantar fascia acts as a shock-absorber and supports the arch of the foot. If tension and stress on the fascia become too great, small tears can occur that cause irritation of the fascia.
Although plantar fasciitis is traditionally thought to be caused by inflammation, some medical experts now believe degeneration is a more likely cause, because of the absence of inflammatory cells within the fascia of some patients.
What are the Symptoms of Plantar Fasciitis?
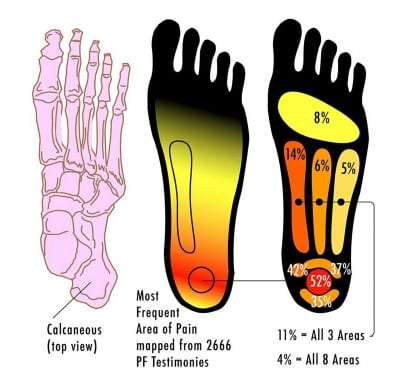
The pain of plantar fasciitis typically begins slowly, usually in the heel of the foot, typically causing a stabbing pain in the bottom of the foot near the heel. Occasionally, though, the onset of pain is sudden when missing a step, or after jumping from a height and landing on the feet.
The pain from plantar fasciitis may radiate from the heel forward, resulting in foot arch pain. There may also be a tenderness in the sole of the foot and on the inside of the heel, when pressing on that part of the foot. The pain can range from slightly uncomfortable to very painful, depending on how badly the fascia is damaged.
The pain is usually the worst with the first few steps after awakening from sleep. However, the pain can also occur after long periods of standing, or when rising from sitting. The pain can also be more severe when climbing stairs. The degree of discomfort can sometimes lessen with activity during the day or after warming up, but it can become worse when undertaking prolonged or vigorous activity. Most patients describe the pain as being worse right after exercise, not during it. The pain is often more severe when walking in bare feet, or when wearing shoes with minimal support.
How is Plantar Fasciitis Diagnosed?
The diagnosis of plantar fasciitis is based on the patient’s medical history (past injuries and illnesses), along with a simple physical examination. The medical history questions will include asking about the types of physical activity in which the patient engages. The exam includes checking for areas of tenderness in the foot to determine the cause. Typically, there is tenderness at the bottom of the inner heel where the plantar fascia attaches. The exam also includes observing how the patient stands and walks.
X-rays are not helpful in diagnosing plantar fasciitis because an x-ray does not clearly show ligaments. However, an X-ray will show a stress fracture, bone cyst, a pinched nerve, and other foot or ankle bone problems that might be present and can cause symptoms similar to plantar fasciitis. X-rays will also show if there is a bone spur on the heel; however, a bone spur does not necessarily mean plantar fasciitis is causing the pain.
How is Plantar Fasciitis Treated?
Most patients suffering plantar fasciitis pain recover with conservative treatments within several months by resting, icing the painful area, and stretching. However, there is not a single treatment that provides universal relief. When treating plantar fasciitis, reducing pain and inflammation is the priority.
Initial treatments:
- Rest feet by cutting back on activities that make the foot hurt.
- Avoid walking or running on hard surfaces.
- An over-the-counter pain reliever like ibuprofen (e.g., Advil or Motrin) or naproxen (e.g., Aleve).
- PRICE principle (Protection, Rest, Ice, Compression, and Elevation) to help reduce pain and inflammation. When applying ice or a cold therapy wrap, limit the application to 20 minutes, three or four times a day. Ice should not be applied directly to the skin but through a wet towel to avoid skin burns. Commercial gel packs and wraps are a convenient method of application.
- Taping the foot is an excellent way to relieve pain. It helps reduce some of the strain on the plantar fascia, allowing the tissues to heal. It may need to be regularly applied until symptoms resolve, but many people notice an immediate improvement.
- Massaging the plantar fascia by rolling the bottom of the foot on a tennis ball can be helpful.
Therapies:
Stretching and strengthening exercises, or using specialized devices may provide symptom relief.
- Physical therapy. Under the supervision of a physical therapist, the patient can perform exercises like toe stretches, calf stretches and towel stretches (pull on both ends of a rolled towel that is under the ball of the foot) several times a day. These exercises stretch the plantar fascia and Achilles tendon and can strengthen lower leg muscles that stabilize the ankle and heel. A therapist can also instruct patients in the proper technique for applying athletic tape to help support the foot.
- Night splints. A physical therapist or doctor might recommend wearing a splint that stretches the calf and foot arch while sleeping. The splint holds the plantar fascia and Achilles tendon in a lengthened position overnight and helps prevent the arch of the foot from tightening up.
- Orthotics. Custom fitted and off-the-shelf arch supports (orthotics) can help distribute pressure on the feet more evenly. Use orthotics in both shoes, even if only one foot has plantar fasciitis pain.
- New shoes. Sometimes, a new pair of shoes with good arch support and a cushioned sole may be all that is required to stop the pain resulting from plantar fasciitis.
Other procedures:
After several months, if more conservative measures do not help, the following procedures are helpful.
- Injections. Injecting a type of steroid medication into the tender area may provide temporary pain relief. Multiple injections are not given because they can weaken the plantar fascia, and possibly cause it to rupture.
- Extracorporeal shock wave therapy. The use of sound waves in the area of heel pain can help stimulate healing. This process may work for chronic plantar fasciitis that hasn’t responded to more conservative treatments. This procedure might cause bruising, swelling, numbness, tingling, or even additional pain. Some studies show promising results, but it hasn’t been shown to be consistently effective.
- Tenex procedure. This minimally invasive procedure removes the scar tissue of plantar fasciitis without surgery.
Surgery:
In some cases, surgery is needed to relieve severe pain and allow the patient to return to normal activities.
- Surgery. Few people (around 5%) need surgery to detach the plantar fascia from the heel bone. It’s an option only when the pain is severe, and all else fails. However, the success rate is only about 70-80%. Side effects include a weakening of the arch of the foot. Complications can include nerve damage, fallen arches, infection, and ongoing symptoms. Doctors only suggest it for people who still have pain after trying other treatments for 6 to 12 months. If the surgery is successful, the recovery period is 9 to 12 weeks.
What are the Plantar Fasciitis Risk Factors?
Although the pain of plantar fasciitis can arise without an apparent cause, factors that can increase the risk of developing plantar fasciitis include:
- Certain types of exercise. Activities that place a lot of stress on the heel and attached tissue, such as long-distance running, jumping, ballet, and aerobic dance can contribute to the onset of plantar fasciitis.
- Foot mechanics. Being flat-footed, having a high arch, or even having an abnormal pattern of walking can affect the distribution of weight when standing, which places additional stress on the plantar fascia.
- Obesity. Excess weight puts extra stress on the plantar fascia.
- Occupations requiring standing. Factory workers, teachers, and others who spend most of their work hours walking or standing on hard surfaces can damage their plantar fascia.
Plantar fasciitis most often occurs because of injuries that have happened over time. With treatment, the pain will subside within a few weeks. But it may take a few months to even a year before the pain is completely gone. The good news is plantar fasciitis typically responds to medications and conservative treatment measures. However, plantar fasciitis pain that doesn’t go away can indicate an underlying disease or complications, such as a tear of the plantar fascia.
Ignoring plantar fasciitis may result in chronic heel pain that may eventually hinder regular activities. For example, changing the way of walking to minimize plantar fasciitis pain can lead to foot, knee, hip, or back problems.
Novus Spine & Pain Center
Novus Spine & Pain Center is in Lakeland, Florida, and specializes in treating pain resulting from Plantar Fasciitis. By using a comprehensive approach and cutting edge therapies, we work together with patients to restore function and regain an active lifestyle, while minimizing the need for opiates.
To schedule an appointment, please contact us online, request a call back, or call our office at 863-583-4445.
Plantar Fasciitis Resources
Plantar Fasciitis (WebMD)
Plantar Fasciitis (Mayo Clinic)
Plantar Fasciitis (Sports Injury Clinic)
Plantar Fasciitis (American Orthopaedic Foot & Ankle Society)
Plantar Fasciitis (Johns Hopkins)
Plantar Fasciitis Treatment (Wikipedia)
Tenex Patient Info (Tenex Fast Procedure)
Updated: May 12, 2020

