Your Achilles tendon is a strong, fibrous cord that connects the muscles in your calf to your heel bone and plays a crucial role in everyday movements. But when this tendon becomes inflamed, it can lead to a painful condition known as Achilles tendinitis.
Achilles tendinitis is a common overuse injury that affects people of all ages and activity levels. Whether you’re a seasoned athlete or just someone who enjoys walking, understanding this condition is key to preventing and managing it effectively. This guide will provide valuable insights into Achilles tendinitis, including its causes, symptoms, treatment options, and prevention strategies.
In This Article:
- Key Takeaways
- What is the Achilles Tendon
- What is Achilles Tendinitis?
- Causes and Risk Factors
- Recognizing the Symptoms
- Potential Complications
- Prevention Strategies
- Treatment Options
- Living with Achilles Tendinitis
- FAQ
- What is Achilles tendinitis?
- What are the symptoms of Achilles tendinitis?
- What causes Achilles tendinitis?
- Who is at risk for Achilles tendinitis?
- How is Achilles tendinitis diagnosed?
- What are the treatment options for Achilles tendinitis?
- How can I prevent Achilles tendinitis?
- What are the complications of Achilles tendinitis?
- When should I see a pain doctor for Achilles tendinitis?
- What is the long-term outlook for people with Achilles tendinitis?
- Conclusion
- Novus Spine & Pain Center
- Additional Resources
Key Takeaways
- Achilles Tendinitis is a Common Overuse Injury. The injury affects the tendon that connects your calf muscles to your heel bone.
- Recognize the Symptoms: Pain, stiffness, and swelling at the back of the heel, especially after activity or in the morning.
- Understand the Causes: Overuse, sudden increases in exercise intensity, improper footwear, and tight calf muscles.
- Know the Risk Factors: Age, gender, certain medical conditions, and specific sports activities.
- Prevent Achilles Tendinitis: Gradually increase exercise intensity, wear proper footwear, stretch regularly, and maintain a healthy weight.
- Seek Medical Attention: You should see a pain management specialist if you experience persistent pain or difficulty bearing weight.
- Treatment Options Vary: Rest, ice, compression, pain medication, physical therapy, and, in severe cases, surgery.
- Most People Recover Fully: With proper treatment, care, and management, you can expect a full recovery.
- Return to Activity Gradually: Avoid re-injury by slowly returning to your regular routine.
- Maintain Long-Term Tendon Health: Healthy lifestyle choices and preventive measures can help avoid future injury to the Achilles tendon.
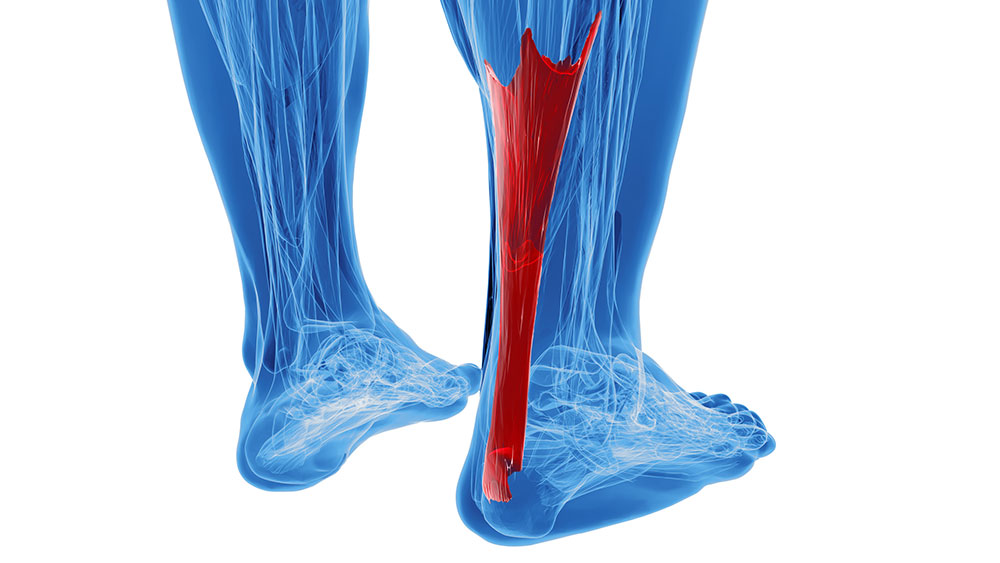
What is the Achilles Tendon?
The Achilles tendon is the largest and strongest tendon in the body. It connects the calf muscle to the heel bone and plays a crucial role in walking, running, and jumping. It is made up of thousands of collagen fibers, which are strong and flexible. These fibers are arranged in parallel bundles, which gives the tendon its strength.
When the calf muscle contracts, it pulls on the Achilles tendon, which in turn causes the heel bone to move upward, which is essential for walking, running, and jumping.
What is Achilles Tendinitis?
Achilles tendinitis is an inflammation of the Achilles tendon. The inflammation is what causes pain.
Causes of Achilles Tendinitis
Achilles tendinitis is most commonly caused by overuse, such as:
- Sudden increase in exercise intensity or duration.
- Repetitive strain from activities like running, jumping, or dancing.
- Improper footwear.
- Tight calf muscles.
Other risk factors for Achilles tendinitis include:
- Age (more common in middle age).
- Gender (more common in men).
- Certain medical conditions (diabetes, obesity, rheumatoid arthritis).
Symptoms of Achilles Tendinitis
The most common symptoms of Achilles tendinitis include:
- Pain and stiffness in the back of the heel, especially in the morning or after exercise.
- Swelling and tenderness at the back of the heel.
- Thickening of the tendon.
- Limited range of motion in the ankle.
Diagnosis of Achilles Tendinitis
A pain doctor will diagnose Achilles tendinitis by performing a physical examination and reviewing your medical history. They may also order imaging tests, such as an X-ray or ultrasound, to rule out other conditions.
Treatment of Achilles Tendinitis
Treatment for Achilles tendinitis typically involves rest, ice, compression, and pain medication. In some cases, physical therapy may also be recommended. In severe cases, surgery may be necessary.
Causes and Risk Factors
Achilles tendinitis is an overuse injury most common in runners and other athletes who participate in activities that involve repetitive stress on the Achilles tendon. The tendon is a thick band of tissue connecting the calf muscle to the heel bone. When the tendon is repeatedly stressed, it can become inflamed and painful.
Common Causes
- Overuse: The most common cause of Achilles tendinitis is overuse. This can occur from suddenly increasing the intensity or duration of your workouts or participating in activities that stress your Achilles tendon, such as running, jumping, or dancing.
- Improper Footwear: Wearing shoes that are too tight or loose can also contribute to Achilles tendinitis.
- Tight Calf Muscles: Tight calf muscles can put extra stress on the Achilles tendon.
- Sudden increase in exercise intensity or duration: If you suddenly increase the intensity or duration of your workouts, you may be at increased risk for Achilles tendinitis.
- Repetitive Strain from Activities Like Running, Jumping, or Dancing: If you participate in activities that put a lot of stress on your Achilles tendon, you may be at increased risk for Achilles tendinitis.
Risk Factors
Several factors can increase your risk of developing Achilles tendinitis, including:
- Age: The risk of Achilles tendinitis increases with age. This is because the tendon becomes less flexible and more prone to injury as you age.
- Gender: Men are more likely to develop Achilles tendinitis than women.
- Activity Level: People active in sports or other activities that put a lot of stress on the Achilles tendon are at increased risk for Achilles tendinitis.
- Certain Medical Conditions: People with certain medical conditions, such as diabetes and rheumatoid arthritis, are also at increased risk for Achilles tendinitis.
Recognizing the Symptoms
The pain associated with Achilles tendinitis typically begins as a mild ache in the back of the leg or above the heel after running or other sports activity. Episodes of more severe pain may occur after prolonged running, stair climbing, or sprinting. You might also experience tenderness or stiffness, especially in the morning, which usually improves with mild activity.
The pain may be a mild ache or more severe, depending on the extent of the injury and the type of activity that is causing the pain. If the pain or disability is severe, you may have a torn (ruptured) Achilles tendon and should seek immediate medical attention.
Potential Complications
If left untreated or poorly managed, Achilles tendinitis can significantly increase the risk of further complications in the affected leg and ankle. These complications can include:
- Tendon Rupture: The most serious complication of Achilles tendinitis is a complete tear (rupture) of the Achilles tendon. This often occurs when a weakened tendon is subjected to sudden, forceful stress. A rupture is characterized by a sudden, sharp pain in the back of the heel and often a popping or snapping sensation. Surgical intervention is typically required to repair a ruptured Achilles tendon.
- Chronic Tendinopathy: If Achilles tendinitis is not managed correctly, it can become a chronic condition characterized by persistent pain, stiffness, and decreased mobility. This can significantly impact your ability to participate in physical activities and affect your overall quality of life.
- Heel Pain (Bursitis): Even after the initial inflammation subsides, some individuals may experience ongoing pain in the heel or back of the leg. Inflammation of the bursa, a fluid-filled sac located near the Achilles tendon, can occur due to persistent irritation from Achilles tendinitis. This condition can cause pain and swelling at the back of the heel due to scar tissue formation, thickening of the tendon, or other related conditions.
- Decreased Mobility and Function: Achilles tendinitis can limit your ability to perform daily activities that involve walking, running, or climbing stairs. This can lead to decreased physical activity and a decline in overall fitness.
- Plantar Fasciitis: The altered biomechanics and gait patterns resulting from Achilles tendon pain can lead to heel pain (plantar fasciitis).
It’s important to seek medical attention if you experience persistent pain or other symptoms associated with Achilles tendinitis. Early diagnosis and appropriate treatment can help prevent these complications and improve your chances of a full recovery.
Prevention Strategies
Achilles tendinitis is a common overuse injury that can be prevented with simple lifestyle changes and preventative measures. To reduce the risk of developing Achilles tendinitis, individuals can use some of the strategies listed here to help reduce the likelihood of overuse injuries.
Gradual Increase in Exercise Intensity and Duration
One of the most important things you can do to prevent Achilles tendinitis is gradually increasing your workout intensity and duration. This is especially important if you are starting a new exercise program or returning to exercise after a period of inactivity. When you gradually increase your activity level, you give your body time to adjust to the new demands.
Proper Footwear
Wearing proper footwear can also help to prevent Achilles tendinitis. Shoes should fit well and provide adequate support and cushioning. It is essential to choose shoes that are appropriate for the type of activity you will be doing. For example, running shoes are designed to absorb shock and provide stability, while walking shoes are designed to provide support and comfort.
Stretching and Strengthening Exercises
Regular stretching and strengthening exercises can help to improve flexibility and muscle strength, which can help to reduce your risk of Achilles tendinitis. It is important to stretch your calf muscles before and after exercise. You can also strengthen your calf muscles by doing exercises such as calf raises and heel drops.
Maintaining a Healthy Weight
Excess weight can put additional stress on your Achilles tendon, so it is important to maintain a healthy weight. If you are overweight or obese, talk to your pain specialist about ways to lose weight safely and effectively.
Rest and Recovery
Resting and including recovery days in your training schedule is essential. This will give your body time to repair itself and prevent overuse injuries.
Avoiding Sudden Changes in Activity
Avoid sudden changes in your activity level. If you need to increase the intensity or duration of your workouts, do so gradually.
If you experience any pain in your Achilles tendon, seeing a pain management professional for diagnosis and treatment is essential. Early treatment can help to prevent the condition from worsening.
Additional Tips
- Warm up and cool down properly before and after exercise.
- Wear ankle braces or heel cups if recommended by your pain doctor.
- Avoid activities that put a lot of stress on your Achilles tendon, such as running on hard surfaces or jumping.
- If you have pain in your Achilles tendon, stop exercising and see a pain management specialist.
By following these tips, you can help to reduce your risk of Achilles tendinitis and stay active and healthy.
Treatment Options
Treatment for Achilles tendinitis typically involves a combination of rest, ice, compression, and pain medication. In some cases, physical therapy may also be recommended. In severe cases, surgery may be necessary.
Non-Surgical Treatment
Non-surgical treatment is the most common approach for Achilles tendinitis. It typically involves the following:
- Rest: Rest is essential for allowing the Achilles tendon to heal. This means avoiding activities that stress the tendon, such as running, jumping, or playing sports. You may need crutches or a walking boot to take pressure off the tendon.
- Ice: Applying ice to the affected area for 15-20 minutes at a time, several times a day, can help to reduce pain and inflammation.
- Compression: Wearing a compression bandage or brace can help to support the Achilles tendon and reduce swelling.
- Pain Medication: Over-the-counter pain medications, such as ibuprofen or acetaminophen, can help to relieve pain and inflammation.
In some cases, physical therapy may also be recommended. Physical therapy can help to improve flexibility, strength, and range of motion in the ankle and calf muscles. A physical therapist can also teach you how to properly use crutches or a walking boot and safely return to activity.
Surgical Treatment
Surgery is typically only recommended for Achilles tendinitis that does not improve with non-surgical treatment. Several surgical procedures can be used to treat Achilles tendinitis, including:
- Percutaneous Tenotomy: A procedure that involves making small incisions in the Achilles tendon to release scar tissue and improve flexibility.
- Open Tendon Repair: This procedure is used to repair a torn Achilles tendon.
- Minimally Invasive Surgery: Minimally invasive surgery techniques are becoming increasingly popular for treating Achilles tendinitis. These techniques involve making small incisions, which can lead to less pain, scarring, and recovery time.
If you are considering surgery for Achilles tendinitis, it is important to discuss the risks and benefits of the procedure with your pain doctor.
Living with Achilles Tendinitis
Achilles tendinitis can be a frustrating and painful condition, but you can do several things to manage your symptoms and improve your quality of life.
Managing Pain and Discomfort
There are many things you can do to manage pain and discomfort associated with Achilles tendinitis:
- Rest: Rest is essential for allowing the Achilles tendon to heal. Avoid activities that stress the tendon, such as running, jumping, or playing sports.
- Ice: Applying ice to the affected area for 15-20 minutes at a time, several times a day, can help to reduce pain and inflammation.
- Compression: Wearing a compression bandage or brace can help to support the Achilles tendon and reduce swelling.
- Pain Medication: Over-the-counter pain medications, such as ibuprofen or acetaminophen, can help to relieve pain and inflammation.
- Physical Therapy: A physical therapist can teach you exercises to improve flexibility, strength, and range of motion in your ankle and calf muscles.
Returning to Activity
It is important to gradually return to activity after Achilles tendinitis. This means starting with low-impact activities, such as walking or swimming, and gradually increasing the intensity and duration of your workouts as your pain improves. You should also avoid activities that put a lot of stress on your Achilles tendon, such as running on hard surfaces or jumping.
Tips for Returning to Activity
- Start slowly and gradually increase the intensity and duration of your workouts.
- Warm up and cool down properly before and after exercise.
- Wear supportive shoes.
- Listen to your body and stop if you experience any pain.
Long-Term Outlook
Most people with Achilles tendinitis make a full recovery with proper treatment. However, it can take several months for the pain to resolve completely. In some cases, Achilles tendinitis can become chronic, meaning the pain and stiffness may persist for months or even years.
If you experience chronic Achilles tendinitis, there are some things you can do to manage your symptoms and improve your quality of life. These include:
- Maintaining a Healthy Weight: Excess weight can stress your Achilles tendon.
- Stretching and Strengthening Exercises: Regular stretching and strengthening exercises can help to improve flexibility and muscle strength, which can help to reduce pain and improve function.
- Avoiding Activities That Put a Lot of Stress on Your Achilles Tendon: This may include running on hard surfaces, jumping, or playing high-impact sports.
- Wearing Supportive Shoes: Shoes that provide good arch support and cushioning can help to reduce pain.
- Using Orthotic Inserts: Orthotic inserts can help to support your arch and reduce stress on your Achilles tendon.
- Physical Therapy: A physical therapist can teach you exercises to improve flexibility, strength, and range of motion in your ankle and calf muscles.
Talk to your pain management specialist if you have any questions about living with Achilles tendinitis.
FAQs
What is Achilles tendinitis?
Achilles tendinitis is an overuse injury that causes inflammation and pain in the Achilles tendon, a strong, fibrous cord that connects the muscles in your calf to your heel bone. This tendon is essential for walking, running, jumping, and climbing stairs. When inflamed, it can cause significant pain and stiffness, making it difficult to perform everyday activities.
Achilles tendinitis is typically caused by repetitive strain and overuse, often seen in runners and athletes who participate in activities that stress the tendon. Factors such as sudden increases in exercise intensity, improper footwear, and tight calf muscles can also contribute to its development. The condition is characterized by pain and stiffness along the back of the heel, especially in the morning or after exercise. Swelling, tenderness, and thickening of the tendon may also be present.
What are the symptoms of Achilles tendinitis?
Achilles tendinitis typically causes pain and stiffness along the Achilles tendon at the back of the heel. This discomfort generally is worse in the morning or after periods of inactivity, and it often intensifies after exercise or strenuous activity. You may also experience tenderness to the touch and swelling in the area.
In some cases, the tendon itself may feel thickened or nodular. As the condition progresses, you might notice decreased flexibility in your ankle, making it difficult to point your toes or flex your foot. If left untreated, the pain can become persistent and interfere with your ability to perform daily activities, such as walking or climbing stairs.
What causes Achilles tendinitis?
Achilles tendinitis is primarily an overuse injury that develops from repetitive strain and stress on the Achilles tendon. This commonly occurs due to a sudden increase in exercise intensity or duration, especially in running, jumping, or pivoting activities. Individuals participating in sports like basketball, tennis, or running are at a higher risk.
Other factors contributing to Achilles tendinitis include improper footwear that lacks adequate support, tight calf muscles that place extra strain on the tendon, and biomechanical issues such as flat feet or overpronation. Additionally, certain medical conditions like diabetes and obesity can increase your risk of developing this condition.
Who is at risk for Achilles tendinitis?
While Achilles tendinitis can affect anyone, certain factors increase the likelihood of developing this condition. Individuals who participate in sports or activities that involve repetitive or high-impact movements, such as running, basketball, tennis, and dancing, are at an elevated risk. This is due to the increased stress on the Achilles tendon during these activities.
Other risk factors include age, as the tendon tends to lose elasticity with age; gender, with men being more prone to this condition; having tight calf muscles, which can increase strain on the tendon; and certain medical conditions such as diabetes, obesity, and high blood pressure. Improper footwear that lacks support or cushioning can also contribute to the development of Achilles tendinitis.
How is Achilles tendinitis diagnosed?
Diagnosing Achilles tendinitis typically begins with a thorough physical examination by a physician specializing in pain management. A pain doctor will carefully examine your Achilles tendon, assessing for tenderness, swelling, thickening, and range of motion in your ankle. They may also ask about your symptoms, medical history, and activity levels to understand the potential causes.
Imaging tests may sometimes be recommended to confirm the diagnosis and rule out other conditions. An X-ray can help visualize any bone spurs or calcifications contributing to your pain. An ultrasound or MRI can provide detailed images of the tendon to assess the extent of inflammation or any tears in the tendon.
What are the treatment options for Achilles tendinitis?
Treatment for Achilles tendinitis typically focuses on reducing pain and inflammation while promoting healing of the tendon. Conservative, non-surgical approaches are usually the first line of treatment and often prove effective. These include rest, avoiding activities that aggravate the pain, ice packs applied to the affected area, over-the-counter pain medications like ibuprofen or naproxen, and gentle stretching exercises as advised by your pain management professional or physical therapist.
In some cases, your pain medicine physician may recommend other non-surgical options such as corticosteroid injections, platelet-rich plasma (PRP) therapy, or shockwave therapy. If these conservative measures fail to provide relief or the tendon is severely damaged, surgical intervention may be considered to remove damaged tissue or repair the tendon.
How can I prevent Achilles tendinitis?
Preventing Achilles tendinitis involves a multifaceted approach that focuses on reducing stress and strain on the tendon while promoting its overall health and flexibility. One of the most crucial steps is to gradually increase the intensity and duration of your exercise routines, especially if you’re new to an activity or returning after a break. This allows the tendon to adapt to the demands placed upon it, minimizing the risk of overuse.
Additionally, prioritize proper footwear with adequate cushioning and arch support to reduce the impact on your Achilles tendon during activities. Regularly stretching your calf muscles and Achilles tendon can improve flexibility and reduce tightness, further minimizing stress. Maintaining a healthy weight can also lessen the burden on the tendon. If you experience any pain, stop the activity and rest to prevent further injury.
What are the complications of Achilles tendinitis?
While Achilles tendinitis often responds well to conservative treatment, it’s important to be aware of potential complications that can arise if the condition is not properly managed. One of the most serious complications is an Achilles tendon rupture, which is a complete tear of the tendon. This typically occurs with sudden, forceful movements and often requires surgical repair.
Other potential complications include chronic Achilles tendinopathy, where pain and stiffness persist despite treatment, and tendon degeneration, where the tendon weakens and becomes more susceptible to further injury. In some cases, Achilles tendinitis can also contribute to the development of other foot conditions like plantar fasciitis.
When should I see a pain doctor for Achilles tendinitis?
It’s important to seek medical attention for Achilles tendinitis if your pain is persistent and doesn’t improve after a few days of home care, such as rest, ice, and over-the-counter pain medication. You should also consult a pain doctor if the pain is severe, especially if it’s accompanied by sudden swelling or an inability to bear weight on the affected foot. These could be signs of a more serious injury, such as a tendon rupture.
Additionally, it’s advisable to see a physician specializing in pain management if you have any underlying health conditions, such as diabetes, that could affect your healing process. Early diagnosis and appropriate treatment can help prevent the condition from becoming chronic and reduce the risk of complications.
What is the long-term outlook for people with Achilles tendinitis?
The long-term outlook for individuals with Achilles tendinitis is generally positive, especially when the condition is diagnosed early and treated appropriately. With proper care, which may include rest, physical therapy, and other conservative measures, most people can expect a full recovery and return to their normal activities within a few weeks to months.
However, it’s important to note that some cases may become chronic, with persistent pain and stiffness lasting for an extended period. Factors that can influence the long-term outlook include the severity of the initial injury, individual healing capacity, adherence to treatment recommendations, and any underlying health conditions. Maintaining a healthy lifestyle, including regular exercise and proper footwear, can help prevent recurrence and promote long-term tendon health.
Conclusion
Achilles tendinitis can be a painful and debilitating condition, but with proper care and management, most people make a full recovery. Remember the key takeaways from this article: listen to your body, prioritize gradual exercise progression, choose supportive footwear, and don’t hesitate to seek professional medical advice if you experience persistent pain.
By taking proactive steps to protect your Achilles tendon, you can significantly reduce your risk of injury and enjoy a lifetime of healthy movement.
Novus Spine & Pain Center
Novus Spine & Pain Center is in Lakeland, Florida, and specializes in treating Achilles tendinitis. By using a comprehensive approach and cutting-edge therapies, we work together with patients to restore function and regain an active lifestyle while minimizing the need for opiates.
For your convenience, you may schedule an appointment online, request a call back, or call our office at 863-583-4445.
Additional Resources
Achilles Tendon Injuries (Johns Hopkins)
Achilles Tendinitis (American Academy of Orthopaedic Surgeons)
Achilles Tendinitis (Mayo Clinic)
Achilles Tendinitis (Cleveland Clinic)
Achilles Tendinopathy (Sports Medicine Today)
Updated: January 30, 2025

