 Degenerative disc disease (DDD) is one of the most common causes of low back pain and neck pain, though it is one of the most misunderstood conditions. A diagnosis of “degenerative disc disease” can be alarming, because it sounds like a progressive, threatening disease.
Degenerative disc disease (DDD) is one of the most common causes of low back pain and neck pain, though it is one of the most misunderstood conditions. A diagnosis of “degenerative disc disease” can be alarming, because it sounds like a progressive, threatening disease.
Despite its name, degenerative disc disease is not really a disease, and it is not strictly degenerative. The term “degenerative” does not apply to the symptoms, but rather describes the process of the discs degenerating over time, often due to age.
Intervertebral discs (pads of cartilage) cushion the individual vertebrae (bones making up the spinal column). These discs are soft and compressible, acting as “shock absorbers” and allowing the spine to flex, bend, and twist. As the body ages, wear and tear causes these discs to change, often resulting in pain. The degeneration of a disc in the spine is often the effect of natural, daily stress and minor injuries. However, degenerative disc disease can occur in people as young as 20!
What Is Degenerative Disc Disease?
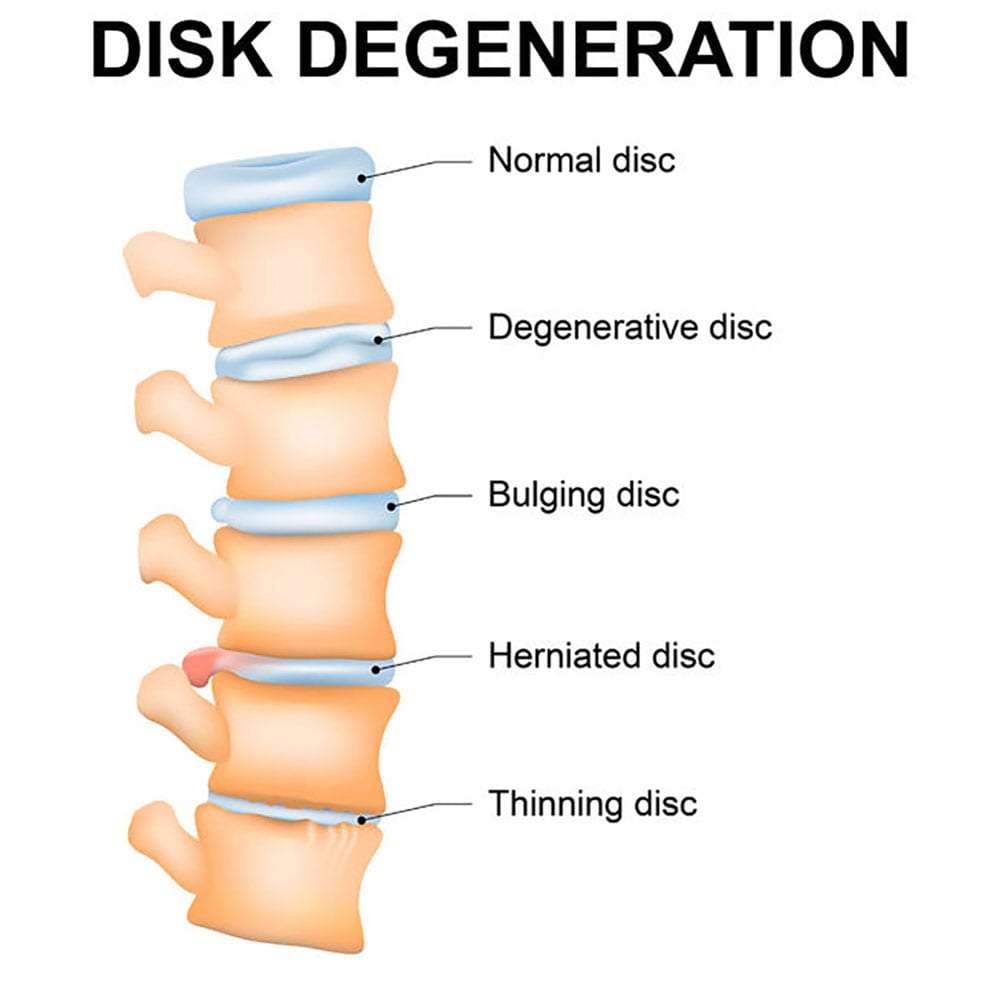
As we age, our intervertebral discs (pillow-like pads between the bones of the spine) lose their flexibility, elasticity, and shock-absorbing characteristics. When this happens, the discs change from a supple, flexible state allowing fluid movement of the spine, to a stiff and rigid state restricting movement.
Symptoms of degenerative disc disease include pain, and possibly radiating weakness or numbness stemming from a degenerated disc in the spine. Degenerative disc disease can take place throughout the spine, but it most often occurs in the discs in the lower back (lumbar region) and the neck (cervical region). The pain from degenerative disc disease also seems to cause reflexive muscle spasms that also cause pain.
What Causes Degenerative Disc Disease?
Although the exact cause of degenerative disc disease is not clear, the majority of evidence seems to indicate it is a result of the normal aging process. At birth, the intervertebral discs are about 80% fluid. As we age, the discs lose fluid, making them less able to absorb shock and force. The reduction of fluid also makes the discs thinner and decreases the distance between the vertebrae.
Sometimes, tiny tears or cracks occur in the outer layer of the disc (annulus) allowing the fluid to escape, causing the disc to bulge or even break open (rupture). If there is enough pressure, it’s possible for the liquid to seep out through the tears in the annulus and cause a herniated disc.
As the disc collapses, both the vertebrae above and below the disc get closer together and have less room to move. The closer the vertebrae are, the more stress they experience. The joints around these bones also experience additional stress. With less space between the vertebrae and a decrease in padding, the spine becomes less stable.
The body may react to the narrowing space and stress between the two vertebrae by creating bone spurs around the disc space to stop excess motion. These bone spurs can grow into the spinal canal and place pressure on the spinal cord and surrounding nerve roots. The pressure will cause pain and affect nerve function (spinal stenosis).
The changes in the disc seem to be more likely to occur among cigarette smokers and people who do demanding physical labor (such as heavy, repetitious lifting). People who are obese also seem more likely to show symptoms of degenerative disc disease. For women, there is substantial evidence that menopause and estrogen loss are responsible for degeneration of the disc in the lumbar (lower) region of the back.
By the age of 60, most people have some level of degenerative disc disease; however, not everyone experiences pain. Injuries can also contribute to degenerative disc disease, as can sports and even regular daily activities. A sudden injury (such as a fall) that leads to a herniated disc can begin the degenerative disc disease process.
What are the Symptoms of Degenerative Disc Disease?
Diagnosis of degenerative disc disease usually consists of an analysis of a patient’s individual medical history, a physical exam designed to reveal muscle weakness, tenderness or poor range of motion, and an MRI to confirm the diagnosis and rule out other causes.
The most useful information to help diagnose degenerative disc disease comes from a complete analysis of the patient’s medical history. The doctor will look at the patient’s symptoms, injuries, and past illnesses. It is helpful to know whether the patient has undergone previous pain treatment. A physical examination checks for muscle weakness, tenderness, and the range of motion. During the physical exam, the doctor will want to know about habits and activities that cause the pain, and the location of the pain.
In the physical exam, the doctor will also:
- Check the affected area’s range of motion.
- Look for which movements cause pain.
- Check for areas of tenderness and any nerve-related changes, such as numbness, tingling, weakness in the affected area, or changes in reflexes.
- Look for any other conditions that might cause the pain, such as fractures, tumors, and infections.
Imaging tests, such as X-rays, are unlikely to help the diagnosis. However, imaging tests can be useful if the symptoms developed after an injury, or there might be nerve damage. In some cases, X-rays may help if the patient’s medical history points to conditions that could affect the spine, such as bone disease, tumors, or infection.
MRIs are useful for detecting damaged discs, but an MRI alone cannot confirm a diagnosis of degenerative disc disease. Diagnostic tests include:
- Magnetic Resonance Imaging (MRI). A magnetic field and radio waves create detailed images of the organs and tissues, which are helpful if there is a concern of a pinched nerve.
- Computed Tomography (CT) Scan. A special X-ray that provides excellent detail of bones.
- Electromyography (EMG). A test of the electrical activity of muscle tissue, using electrodes attached to the skin or inserted into the muscle.
- Nerve Conduction Study (NCS) or Nerve Conduction Velocity (NCV) Test. A test that measures the speed of conduction of an electrical impulse through a nerve. Electrode patches on the skin stimulate a nerve to determine if there is nerve damage or destruction.
How is Degenerative Disc Disease Treated?
There are many treatments available to provide pain relief for degenerative disc disease. However, patients not experiencing severe, debilitating pain should try home treatments first. Physical therapy, specific exercises, and low-impact aerobic conditioning are beneficial in many cases.
The goals for treatment of degenerative disc disease usually include a combination of three areas: pain control, exercise and rehabilitation, and lifestyle modifications.
- Home Treatment Options. Place ice or heat (whichever feels better) on the painful area. Take a pain reliever, such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs, e.g., ibuprofen or naproxen). Do physical therapy and exercises for strengthening and stretching the back.
- Exercise and Rehabilitation. The goal is to help the back heal and to prevent or reduce further recurrences of pain. For patients, exercises are usually best done under the guidance of a physical therapist or other appropriately trained healthcare professional. A side benefit of exercise is that it can also help reduce pain naturally, as it releases endorphins that serve as the body’s natural pain reliever.
- Lifestyle Modifications. This treatment focuses on education to help the patient develop a healthier lifestyle. Often, these changes aim at avoiding stress on the spine and supporting the spine through the right ergonomics and posture. Some home-therapy options include:
-
- Bed rest, but for just a few days. Extended bed rest can further weaken back muscles.
- Restricting activities that increase the pain.
- Light exercise (such as walking, swimming, etc.) under a doctor’s guidance.
Sometimes a combination of treatments such as physical therapy, anti-inflammatory medications like nonsteroidal anti-inflammatory drugs, traction, or epidural steroid injections often provides adequate relief of symptoms.
Generally, non-surgical treatments of degenerative disc disease are successful. However, if more conservative options do not provide relief after two to three months, surgery may be an option. Surgery can be helpful if leg or back pain limits normal activity. Surgery may be an option if there is weakness or numbness in the legs, or if it is difficult for the patient to walk or stand.
There are many surgical options for the treatment of degenerative disc disease. The most common surgical treatments include:
- Anterior Cervical Discectomy and Fusion. A procedure that replaces the intervertebral disc with a small plug of bone or another graft substitute that, in time, fuses the vertebrae.
- Cervical Corpectomy. A procedure that removes a portion of the vertebra and adjacent intervertebral discs to allow for decompression of the spinal cord and nerves. A bone graft, and in some cases a metal plate and screws are used to stabilize the spine.
- Dynamic Stabilization: Following a discectomy, an implant helps offload pressure from the disc by rerouting pressure through the posterior part of the spinal column. As with a fusion, this implant allows mobility to the stabilized segment.
- Facetectomy. A procedure to remove a part of the facet joint to increase space and relieve pressure on a spinal nerve root.
- Foraminotomy. A minimally invasive procedure that enlarges the vertebrae space to increase the size of the nerve pathway. This surgery can be done alone or with a laminotomy.
- Intradiscal Electrothermal Annuloplasty (IDEA) or Intradiscal Electrothermal Therapy (IDET). A minimally invasive technique using heat to contract collagen fibers to deaden nerves irritated by the degeneration. Patients with severely collapsed discs (loss of more than 50% of disc height), or older than 55 are not good candidates for this procedure.
- Intervertebral Disc Arthroplasty, also Artificial Disc Replacement (ADR), or Total Disc Replacement (TDR). A procedure to replace intervertebral discs with artificial ones. This procedure may be a better option for some patients over fusion.
- Laminoplasty. A reconstructive procedure on the cervical (neck) spine to make more room for the spinal cord.
- Laminotomy. A less invasive procedure than conventional vertebral column surgery that removes only a small portion of the posterior part of the spinal ring that covers the spinal cord (lamina) to relieve pressure on the nerve roots.
- Microdiscectomy. A minimally invasive surgical procedure to remove a portion of the inner core of the vertebral disc (nucleus pulposus).
- Percutaneous Disc Decompression. A minimally invasive procedure to reduce or eliminate a small part of a bulging disc by inserting a needle into the disc.
- Spinal Laminectomy. A procedure for treating spinal stenosis by relieving pressure on the spinal cord. The removal (or trimming) of a part of the spinal ring that covers the spinal cord (lamina) to widen the spinal canal and create more space for the spinal nerves.
Other emerging, new treatments are still in beginning clinical trial phases that may prove beneficial to degenerative disc disease patients.
Novus Spine & Pain Center
Novus Spine & Pain Center is in Lakeland, Florida, and specializes in treating pain resulting from degenerative disc disease. By using a comprehensive approach and cutting-edge therapies, we work together with patients to restore function and regain an active lifestyle, while minimizing the need for opiates.
To schedule an appointment, please contact us online, request a call back, or call our office at 863-583-4445.
Degenerative Disc Disease Resources
Degenerative Disc Disease – Fast Facts (VeryWell.com)
Degenerative Disc Disease – Topic Overview (WebMD)
Degenerative changes in the spine: Is this arthritis? (Mayo Clinic)
Degenerative Disc Disease (Wikipedia)
Degenerative Disc Disease (Johns Hopkins)
What is Degenerative Disc Disease (Spine Health)
Degenerative Disc Disease Center (Spine Universe)
Spinal Decompression Therapy (Physical Therapy First)
Intradiscal Electrothermal Therapy (Medscape)
IDET: an Alternative to Invasive Surgery for Chronic Low Back Pain (Spine Health)
Updated: June 18, 2020

